Medicaid Enterprise Analytics
Improving health management for your most at-risk members
With razor-thin margins on reimbursements and more value-based care at-risk contracts, health plans are clamoring for new and innovative ways to address the health of growing Medicaid populations. By mining insights from claim and clinical data, MedeAnalytics provides the foundation for managed care plans and agencies to collaborate and help deliver better outcomes to underserved populations.
Applying data to create person-centered care
Challenge
Solution
Lack of insight into actual impact of social determinants of health within membership limits efficacy of value-based care
Challenge
Solution
Disjointed data sources hinder understanding of member utilization trends and program outcomes
Challenge
Solution
Basic, low-detail view of member health statuses and population patterns stunts plan expansion
Analytics in action
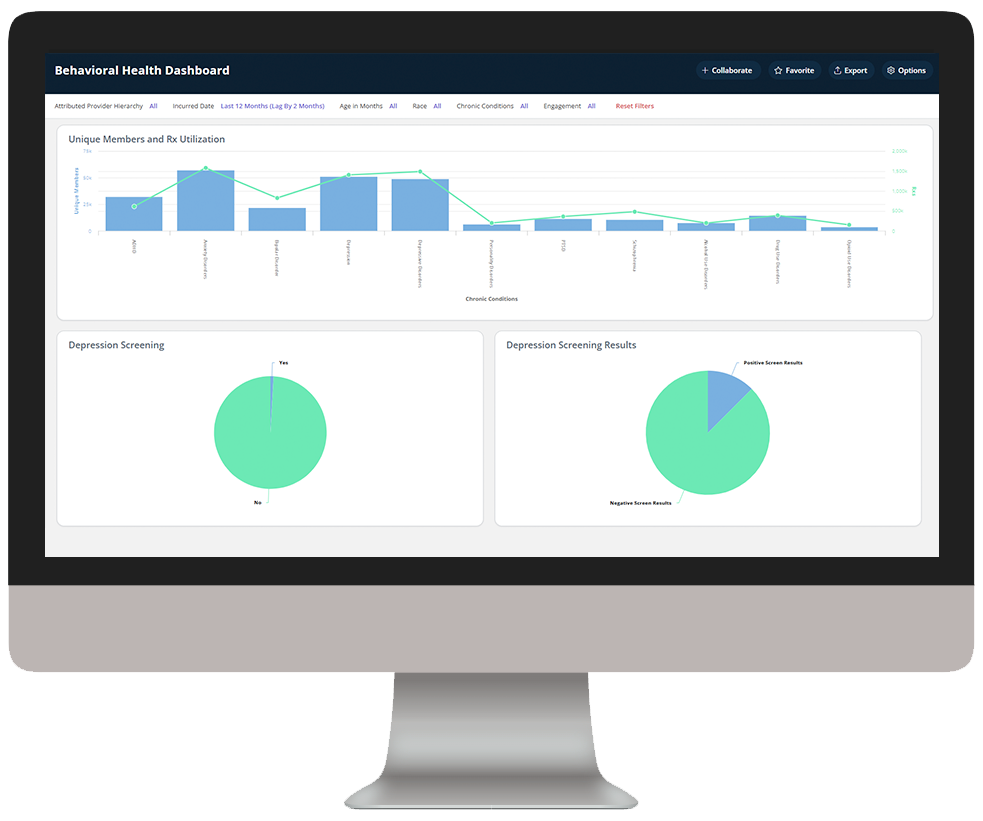
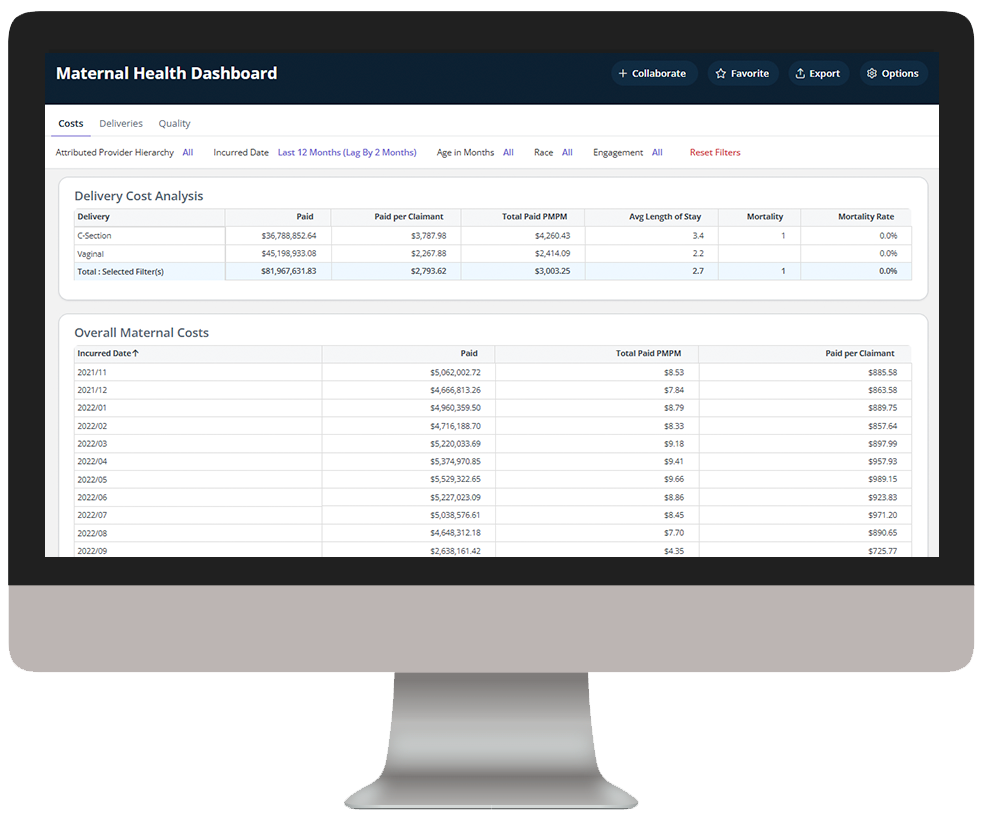
Medicaid Enterprise Analytics delivers key insights into Medicaid beneficiary data, enabling health plans to understand cost drivers, gaps in care, and demographic and SDOH impact to improve care outcomes.
Explore a few key features by hovering over the images below.
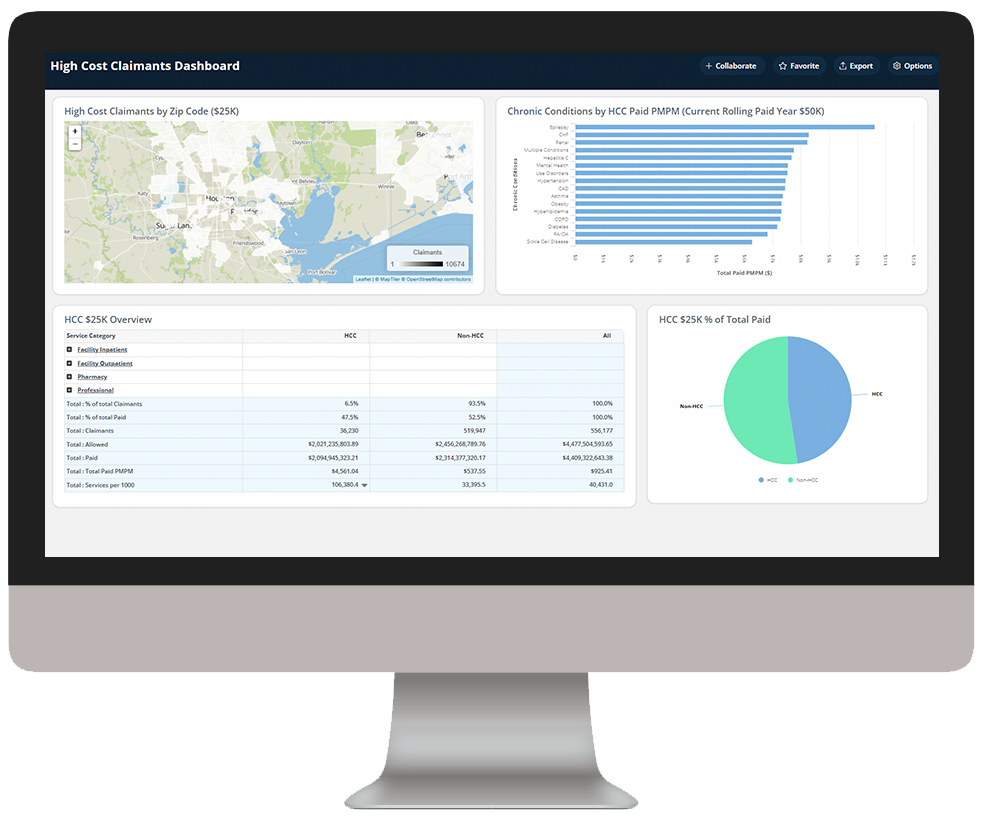
Identify high-cost claimants to prioritize for care management
Dive deeper into Medicaid Enterprise Analytics
Download the data sheet to see how Medicaid Enterprise Analytics integrates traditionally disparate data sources to provide the visibility and transparency health plans need to holistically manage member care.
Get our take on industry trends
Why Healthcare Should “Double-Down” on Exploring AI-powered BI for Reporting
Many areas in healthcare rely not only on the collection of data but, importantly, the ability to decipher and act upon it. In that intersection, reporting was born.
Read on...Why Health Plans and Employers Need Stop Loss Reporting
Due to rising healthcare costs and the Affordable Care Act removing the ban on capitated benefits coverage, numerous employers with self-insured health plans often purchase stop loss coverage. This coverage is not medical insurance; but rather, it’s a financial and risk management tool that protects the employer from excessive claims.
Read on...Bridge the Payer/Provider Data Gap
Every patient has a plethora of data associated with their health record, which can include decades of enrollments, claims, accounts and charges. Much of this data is not housed within the same institutional, facility or provider database…
Read on...Digging deeper: Leveraging analytics to boost service line profitability
Regardless of the size of the hospital or health system, you need to look beyond traditional operational metrics to fully understand your organization’s performance. Insights into revenue, volume, cost, quality and variation across service lines are key to improving both performance and profitability.
Read on...Want to talk with one of our experts?
We're driving data-powered improvement across the industry

Healthcare providers and health systems
Healthcare Providers and Health Systems
use our end-to-end revenue cycle management analytics to lower denials, accelerate A/R, and improve staff productivity.

Healthcare payers and health plans
Healthcare Payers and health plans
deploy our value-based care and provider network analytics to enhance population health, quality and network management and empower their employers and brokers through self-service analytics.

Government Medicare and Medicaid programs
Government Medicare and Medicaid programs
Government Medicare and Medicaid programs rely on our comprehensive dashboards to understand cost drivers, gaps in care, and social determinants impacting beneficiary outcomes.