
Patient Access Insights
Intuitive dashboards and intelligent workflows streamline registration processes
Gaining staff efficiencies, optimizing processes for patient satisfaction, and reducing uncompensated care are critical for modern patient access departments. With intuitive dashboards and automated workflows in a single workspace, your staff can efficiently run patient estimates, improve collections at the point of service, and reduce denials while smoothing out the patient journey.
Deploying analytics to successfully adapt to industry demands
Challenge
Solution
Disparate data collection creates disjointed, expensive and ineffective patient access processes
Challenge
Solution
Insufficient information and human error results in missed collections and bad debt
Challenge
Solution
Limited ability to measure the productivity of remote staff and accuracy of registration tasks
Analytics in action
Our intelligent platform and intuitive user interface make it easy to unlock the value of your data. In as little as three clicks, we bring meaningful insights, powerful visualization and analytics innovation to help you make an even bigger impact at your organization.
Explore a few key features by hovering over the image.
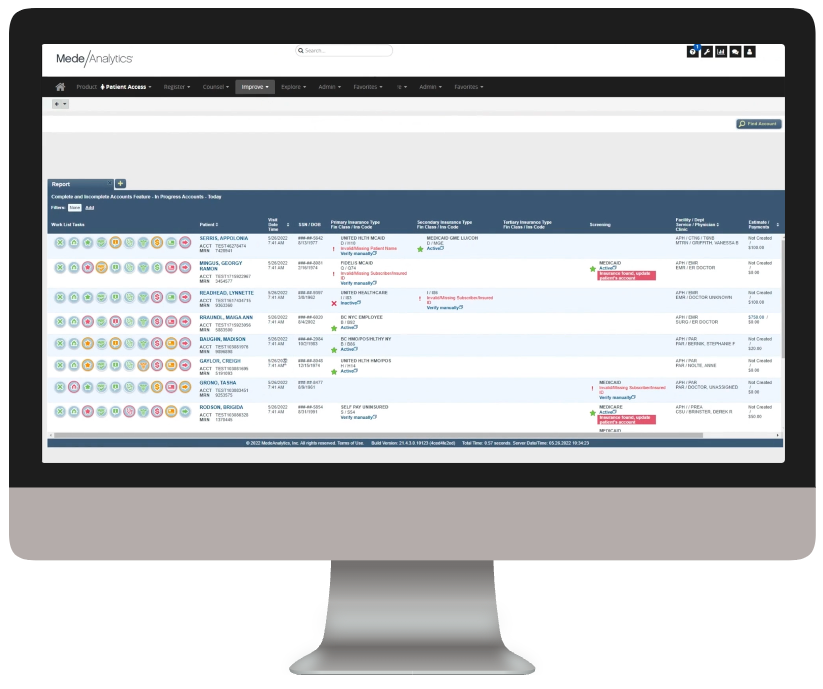
This comprehensive, color-coded worklist consolidates all the important information on the patient into one simple, easy-to-navigate screen
Once you click into a patient, the tool jumps right to unfinished tasks and links straight to relevant information needed to complete the tasks
Many tasks are automated, including prior authorization when possible
Dive deeper into Patient Access
Download the data sheet for next-level details about the transformative effects of Patient Access on your patient engagement, front-office productivity and financial health.
Download the data sheet to see how Productivity Analytics uses data automation to transform your registrar performance.
Get our take on industry trends
Introduction to social risk: What healthcare leaders need to understand
‘Social determinants of health’ has been a common phrase for decades now, but the term social risk is much less…
Read on...AI is your new crystal ball: How predictive analytics can reduce denials
The idea of having a crystal ball to better understand what claims will be denied is an awesome concept. But one we can’t rely on. Thankfully, we have predictive analytics to take the place of a crystal ball.
Read on...3 ways to reduce friction in payer-provider relationships
The dynamic between healthcare providers and payers has historically been quite strained. Though both parties are interested in improving the…
Read on...Position your organization for success under CMS-HCC V28
The transition from CMS-HCC V24 to V28 heralds a significant shift in risk adjustment methodologies and emphasizes improved accuracy and…
Read on...Want to talk with one of our experts?
Provider Value Analytics: Our full lineup of provider solutions
Everything you need to support your front office, mid-cycle and back office.
Patient
Access
Insights
Optimize patient satisfaction during the patient registration and payment clearance processes with critical, real-time analytics information.
Revenue Integrity
Suite
See how clinical operations affect your bottom line with complete visibility into compliance risk and clinical documentation performance.
Business Office
Suite
Achieve optimized cash flow and operational excellence with big-picture insight into opportunities for improving collection rate, denials, and staff productivity.

Workforce Quality Insights
Use powerful analytics capabilities to generate end-to-end insights into how patient access activities are impacting the back-office outcomes.
See the solution ❯
Cost
Insights
Drill down into claims and encounter-level data to target and align controllable costs with outcomes and reimbursement.





