Mede
MedeAdopt
Optimize return on your analytics investments
Analytics solutions require significant investments of time and money—but many health plans are not seeing the returns or effects they'd hoped for. This is often a result of insufficient user adoption, monitoring and ongoing education. MedeAdopt is a self-service tool built to help you ensure that users are extending—rather than limiting—the value and impact of your MedeAnalytics solutions.
Applying data to support your users
Challenge
Solution
Insufficient onboarding and utilization reporting leads to low adoption and engagement
Challenge
Solution
Manual, sparse communications limit user awareness of new features and hinder them from sharing feedback
Analytics in action
MedeAdopt provides real-time, on demand product usage analytics and onboarding, training, and in-app messaging that seamlessly integrate with your analytics solution.
Explore a few key features by hovering over the image.
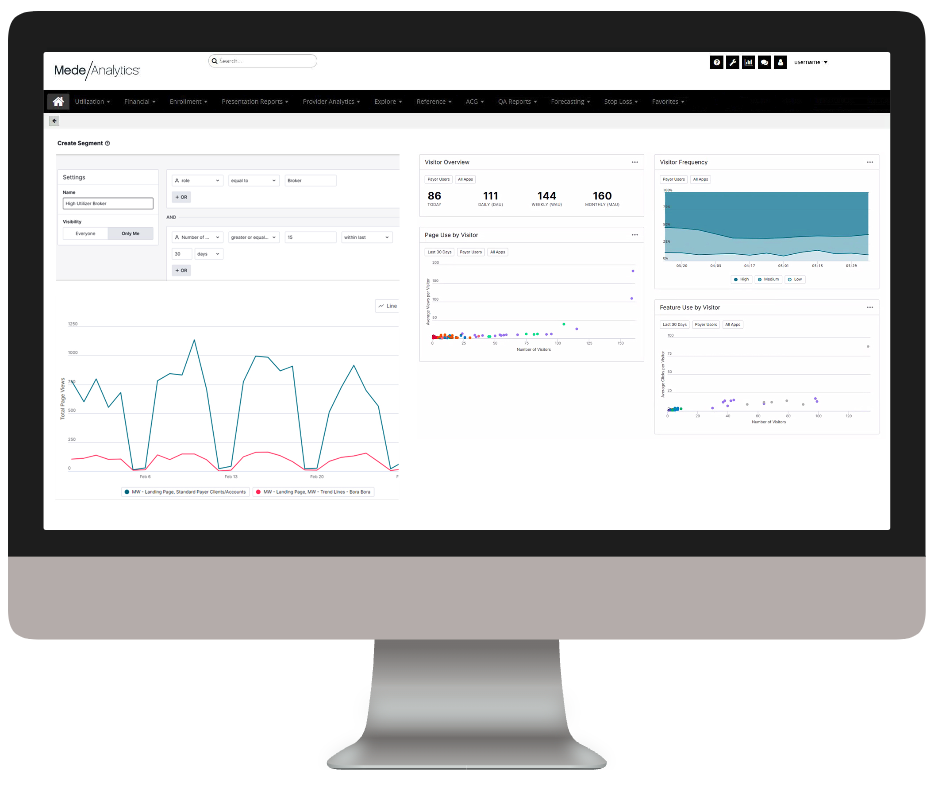
Examine user segments to target training and in-app guides
Find top utilizers and top-used analyses
Get high-level statistics and trends for your users
View user data by page and feature usage
Dive deeper into MedeAdopt
Download the data sheet to see how MedeAdopt gives health plans the data points necessary to inform business decisions and drive user behavior to improve satisfaction, cost savings, communications and engagement.
Explore a few of our most popular resources:
Want to talk with one of our experts?
We're driving data-powered improvement across the industry

Healthcare providers and health systems
Healthcare Providers and Health Systems
use our end-to-end revenue cycle management analytics to lower denials, accelerate A/R, and improve staff productivity.

Healthcare payers and health plans
Healthcare Payers and health plans
deploy our value-based care and provider network analytics to enhance population health, quality and network management and empower their employers and brokers through self-service analytics.

Government Medicare and Medicaid programs
Government Medicare and Medicaid programs rely on our comprehensive dashboards to understand cost drivers, gaps in care, and social determinants impacting beneficiary outcomes.





