Quality Insights
Improve value-based care quality and population health outcomes
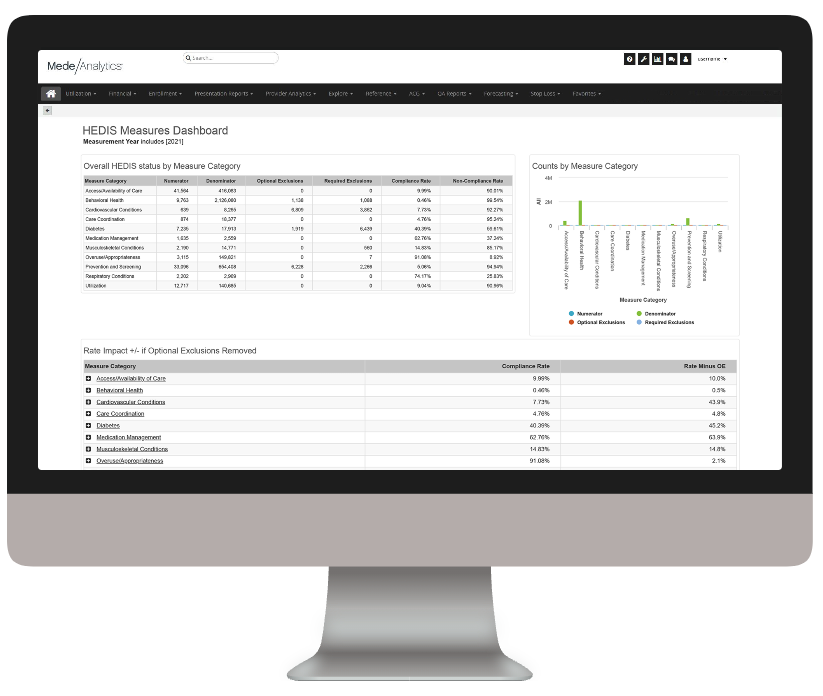
The rise of value-based care has inevitably spurred heightened focus on quality improvement across the healthcare ecosystem. There are two sides to this coin: measures and members. On the measures side, health plans are working to align with strict national standards and state-specific requirements (think: HEDIS, Star ratings). On the members side, payers are striving to understand their patient populations more fully and provide more timely, appropriate interventions.
Delivering comprehensive solutions to enhance performance and outcomes
Challenge
Solution
Siloed, incompatible information from EMRs, claims and other sources hinder efficient quality calculations and data submission
Challenge
Solution
Unnecessary ED visits and readmissions drive up costs and decrease member satisfaction
Challenge
Solution
Insufficient, unreliable data on clinical performance deters provider engagement
Celebrating big wins with Quality Insights
Analytics in action
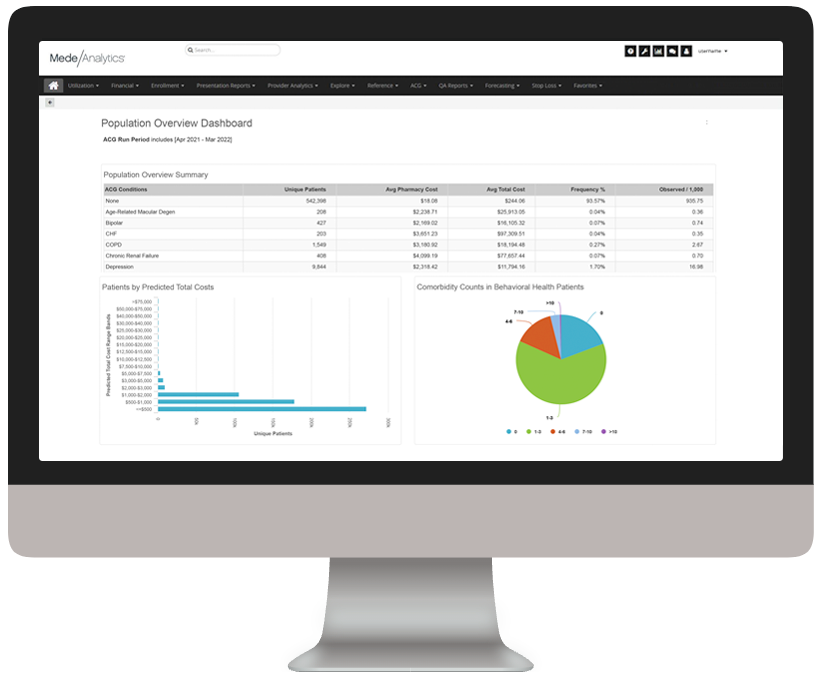
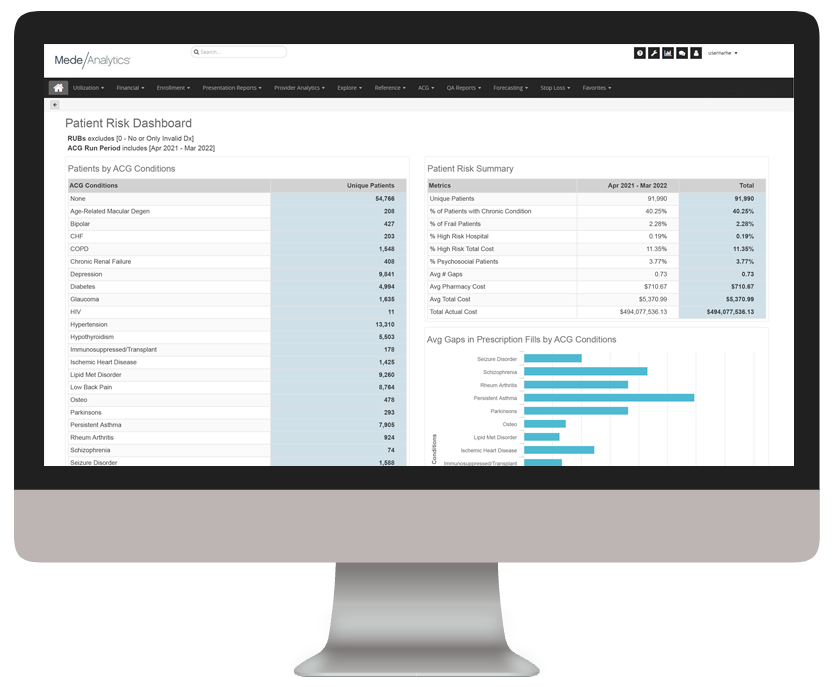
Our intelligent platform and intuitive user interface make it easy to unlock the value of your data. In as little as three clicks, we bring meaningful insights, powerful visualization, and analytics innovation to help you make an even bigger impact at your organization.
As you click through our example dashboards, hover over the image to explore a few key features.
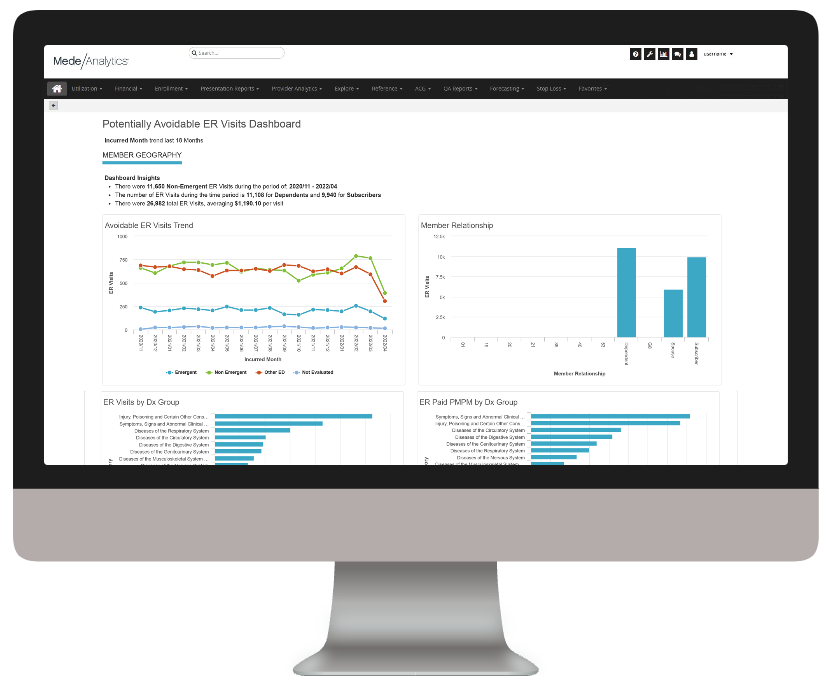
Understand trends in ER utilization
Analyze ER visits by Dx Group
Dive deeper into Quality Insights
Download the data sheet to see how Quality Insights can help your health plan improve care quality and outcomes.
Visit our Value-Based Care Blueprint page for everything you need to know to navigate the intersection of value and analytics.
Get our take on industry trends
Introduction to social risk: What healthcare leaders need to understand
‘Social determinants of health’ has been a common phrase for decades now, but the term social risk is much less…
Read on...AI is your new crystal ball: How predictive analytics can reduce denials
The idea of having a crystal ball to better understand what claims will be denied is an awesome concept. But one we can’t rely on. Thankfully, we have predictive analytics to take the place of a crystal ball.
Read on...3 ways to reduce friction in payer-provider relationships
The dynamic between healthcare providers and payers has historically been quite strained. Though both parties are interested in improving the…
Read on...Adapting nursing education and practice in a post-pandemic, technology-dependent world
Can AI help reduce nurse burnout? What role should nurses play in regulatory conversations? How do clinical training programs incorporate…
Read on...Want to talk with one of our experts?
Payer Value Analytics: Our full lineup of payer solutions
Everything you need to step into the future of healthcare and drive real change across populations.
Quality Insights
Activate insights into population health and quality to improve satisfaction and outcomes for members and maintain a competitive position in the market.
Employer Insights
Elevate data sharing with employer groups to demonstrate plan value and increase efficacy of risk stratification and care management plans.
Network Insights
Accelerate provider performance with evidence-based outcomes comparisons, cost-effectiveness analyses, and extensive segmentation capabilities.