
Did you know that a whopping 30% of the world’s data is healthcare related? 1
Every patient has a plethora of data associated with their health record, which can include decades of enrollments, claims, accounts and charges. Much of this data is not housed within the same institutional, facility or provider database and can be cumbersome and time-consuming to pull together, leaving room for reporting and processing errors. Finding ways to aggregate patient data and maintain it in one place is important because it creates the ability to have immediate, actionable insights, which allows payers and providers to make more informed decisions that save time and money and improve patient outcomes.
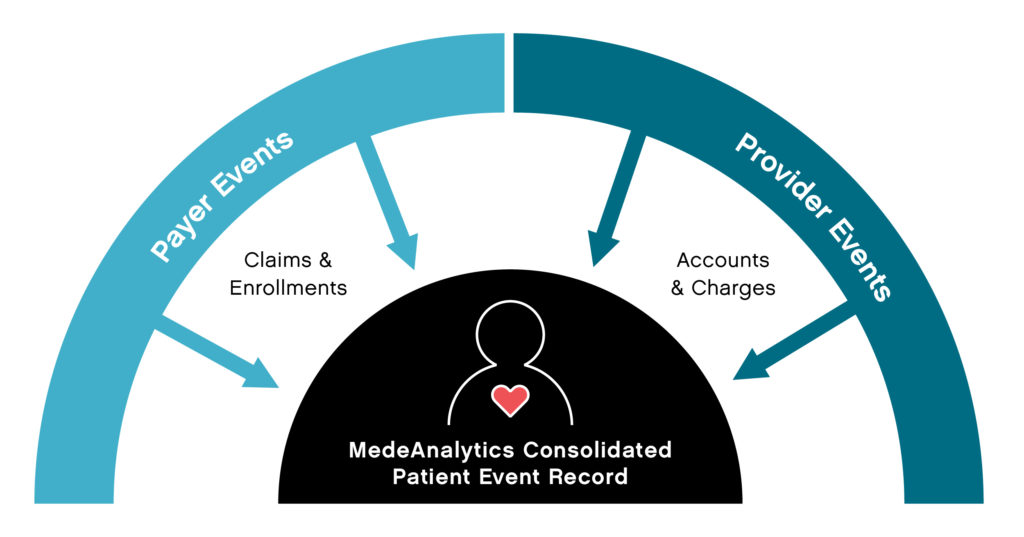
Yet, payers and providers traditionally maintain their own slices of patient data, which include enrollment and claims for payers and accounts and charges for providers. Some data elements are unique to payers and some to providers, but much of it overlaps, referencing the same patient events. By rolling up all pertinent claims for an event and connecting to the accounts and charges, payer and provider data can be linked to a single patient event record.
Linking data in this way allows for more collaboration and cohesive information sharing between payers and providers. Providers get access to data that extends beyond the walls of their organization. Payers get much more timely and complete information on their members, bypassing claim lag times. The new data relationship makes available a whole new set of patient-centric reports that were not possible before. Patient event reporting, for example, can provide true insights into mortality, readmissions, hospital-acquired conditions, which are especially critical to ACOs, IDNs and payvider (provider-owned health plans) organizations.
Succinct collection of data and timely dissemination of actionable insights is essential to enable efficient communications between doctors, hospitals, Accountable Care Organizations (ACOs) and health plans. When data is connected, you can accelerate universal speed to insights so that both payers and providers can make smarter decisions, reduce costs, increase organizational efficacy and improve patient outcomes. Learn more.
Get our take on industry trends
Helping Accountable Care Organizations Navigate the Perfect Storm
In the ever-evolving landscape of healthcare, Accountable Care Organizations (ACOs) find themselves at the epicenter of a transformative era. Recently,…
Read on...Navigating the Medicare Landscape: Implications of the Latest Rule Changes for Healthcare Organizations
The Centers for Medicare & Medicaid Services (CMS) has recently unveiled significant proposed changes to Medicare Advantage (MA), Medicare Prescription…
Read on...Introduction to social risk: What healthcare leaders need to understand
‘Social determinants of health’ has been a common phrase for decades now, but the term social risk is much less…
Read on...AI is your new crystal ball: How predictive analytics can reduce denials
The idea of having a crystal ball to better understand what claims will be denied is an awesome concept. But one we can’t rely on. Thankfully, we have predictive analytics to take the place of a crystal ball.
Read on...


