Blueprint:
How to find success at the intersection of analytics and value
The transition from fee-for-service to value-based payments began as an effort to balance out the United States’ high healthcare spending with its disappointing national health statistics. The New England Journal of Medicine defines value-based care as “a healthcare delivery model in which…providers are rewarded for helping patients improve their health, reduce the effects and incidence of chronic disease, and live healthier lives in an evidence-based way.”
Value-based care ties the amount healthcare providers earn for their services to the results they deliver for their patients, such as the quality, equity and cost of care. Through financial incentives and other methods, value-based care programs aim to hold providers more accountable for improving patient outcomes while also giving them greater flexibility to deliver the right care at the right time.
The COVID-19 pandemic exacerbated and highlighted the need to focus on these five critical components, as it brought heightened attention to clinician burnout (nearly 63 percent reported signs of burnout at the end of 2021) and massive disparities in access to care, quality of care, outcomes, and affordability. The government and regulatory bodies have also played a key part in pushing the value-based care agenda forward with various initiatives (MACRA rule, Value Modifier program, etc.) incentivizing providers to shift away from fee-for-service.
This value-based performance and payment approach has shown signs of moderate success so far by reducing care costs and improving patient outcomes, as well as driving changes in readmission rates, avoidable ED visits, wellness visits, caregiver satisfaction and access to care.
Providers
Value-based care ties the amount providers earn for their services to the results they deliver for their patients. They need to strive for quality and equity at the lowest cost of care.
Payers
In value-based care arrangements, payers must monitor provider performance and member outcomes to manage provider contracts and negotiations.
Mutual key to success
For both payers and providers, succeeding with value-based care means working together to manage population health to improve clinical outcomes of a defined group of individuals through improved care coordination and patient engagement.
Analytics play a critical role in advancing value-based care for a few key reasons:
Empowers data sharing
To succeed, providers need the ability to exchange information between disparate vendors with different interfaces and components. With this interoperability, they can see the full picture of patient and member behaviors and needs.
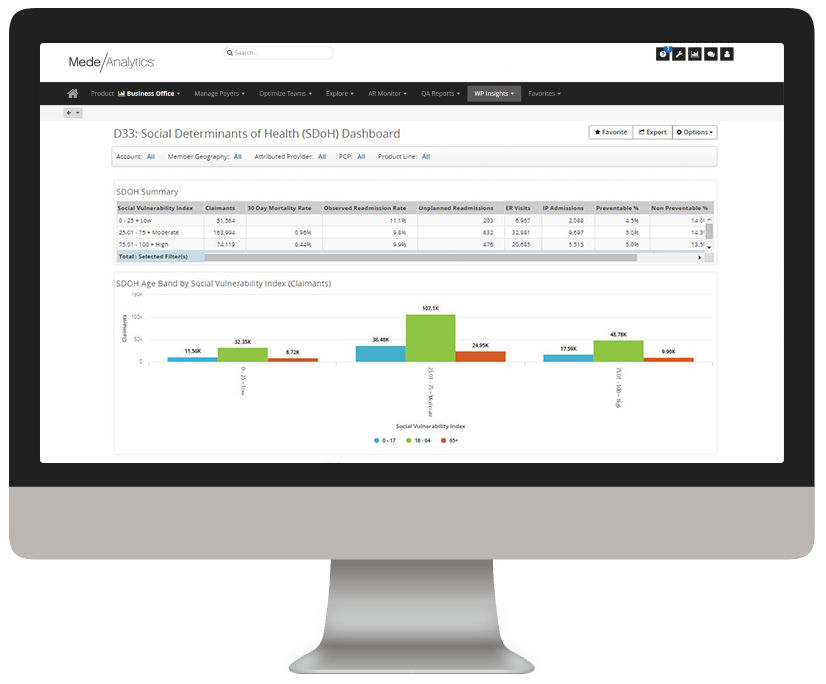
Establishes a 360-degree view of patients
When providers and care managers have a full picture of patient/member behaviors, trends, habits actions and socioeconomic data, they can make informed decisions to positively impact patient and member outcomes.
Integrates claims and clinical data
When previously disconnected data is brought together, it provides unique insight into health outcomes and costs of care. For example, it can be influential in avoiding medication errors and enabling an evidence-based approach to treatment.
Below, you can explore real-life applications of analytics to value-based care using the MedeAnalytics platform.
If you’d like a full demo, let us know.
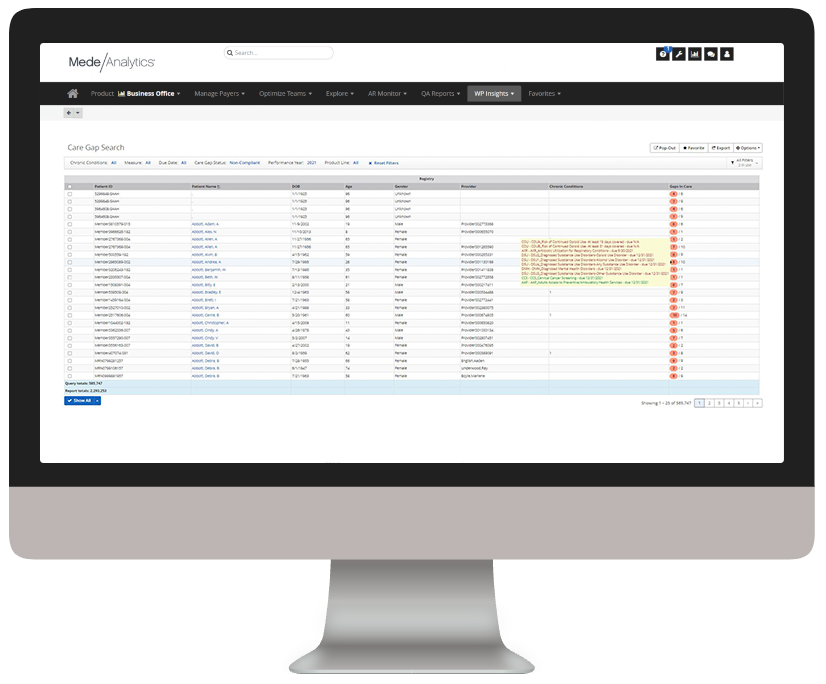
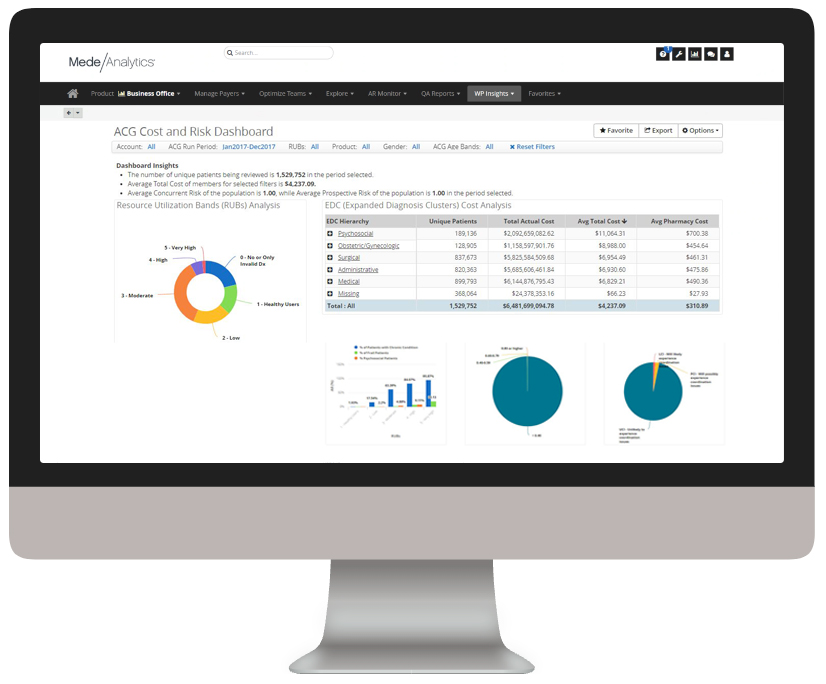
Manage population health and risk
Understand where there are patient care gaps and high-risk groups to help target interventions and programs that improve patient outcomes.
ACGs, chronic conditions, prevention and wellness
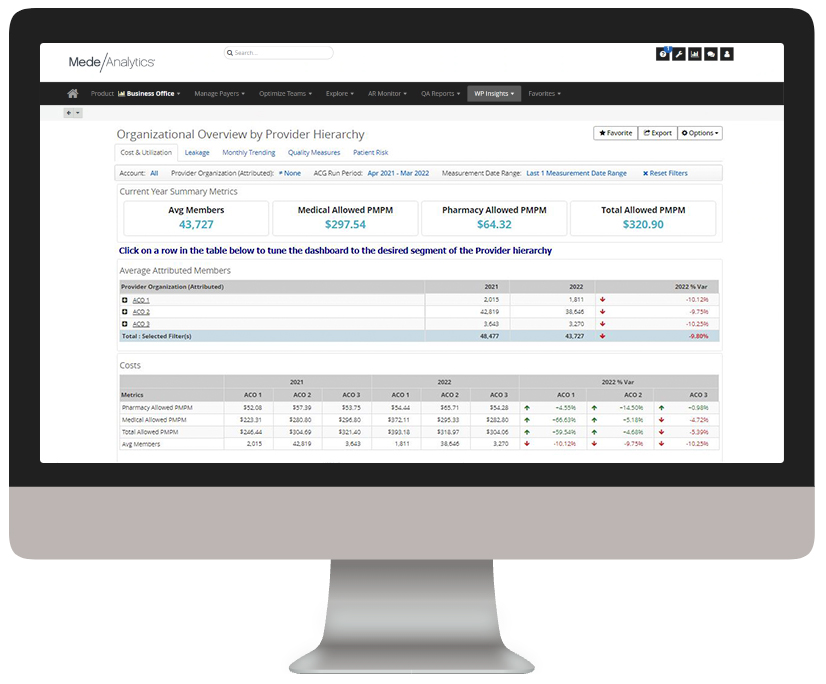
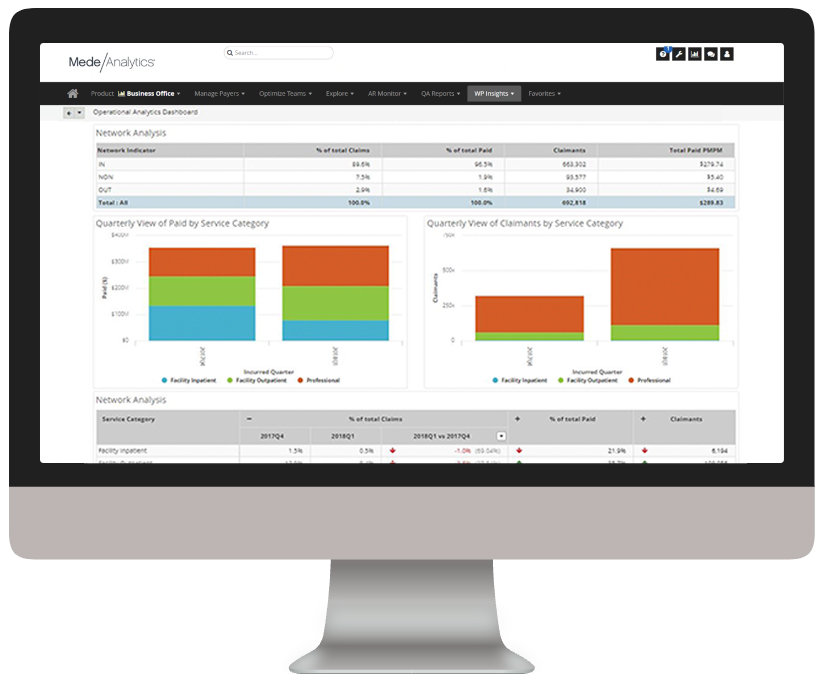
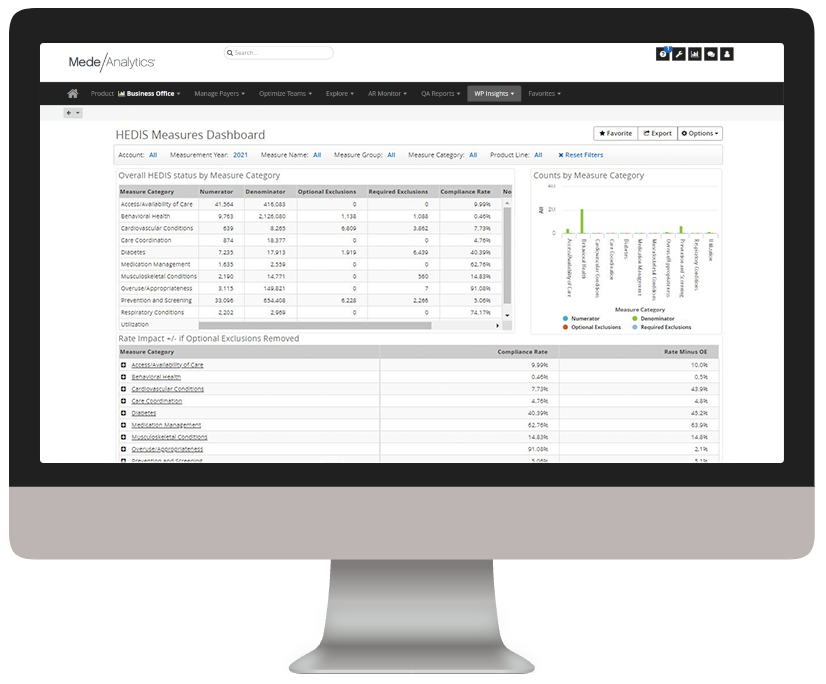
Build high-performing provider networks
Efficiently monitor provider network performance to steer care to select providers, establish tiered-value networks, and improve contracting.
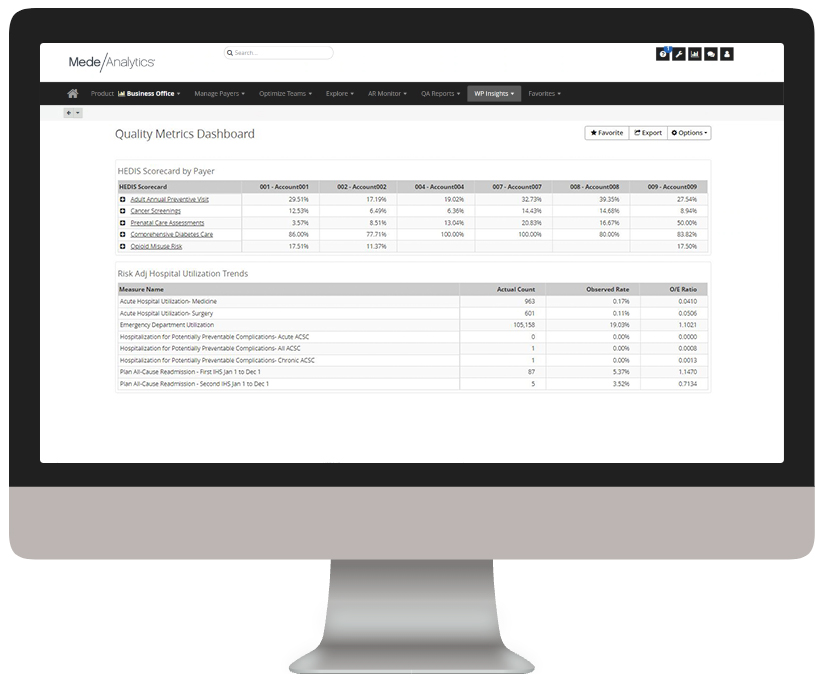
HEDIS, Star, HCAHPS
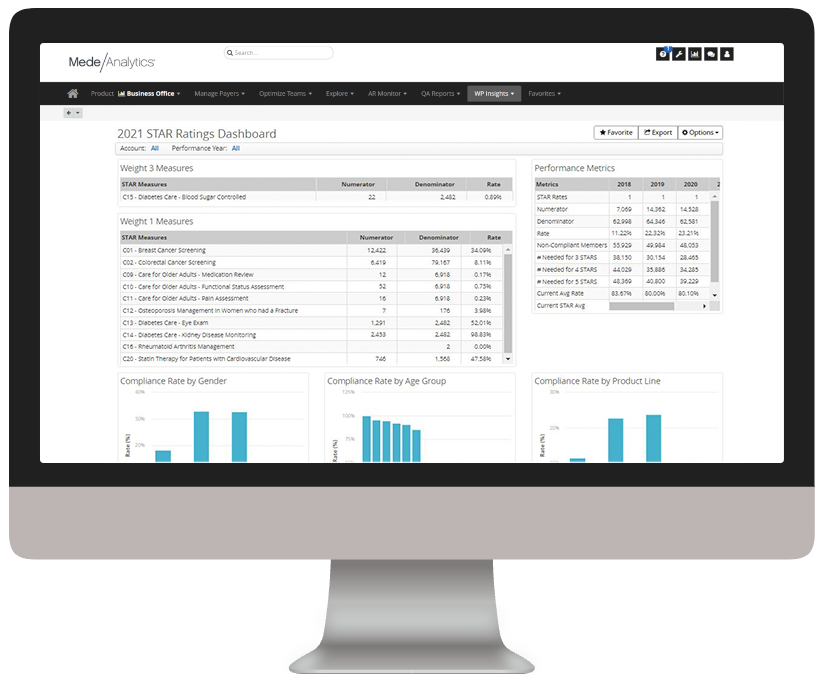
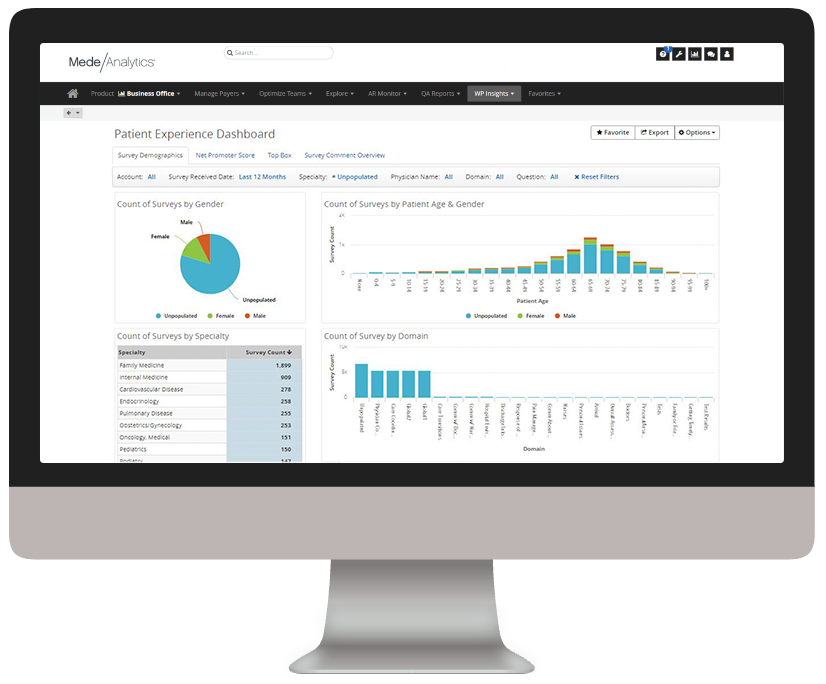
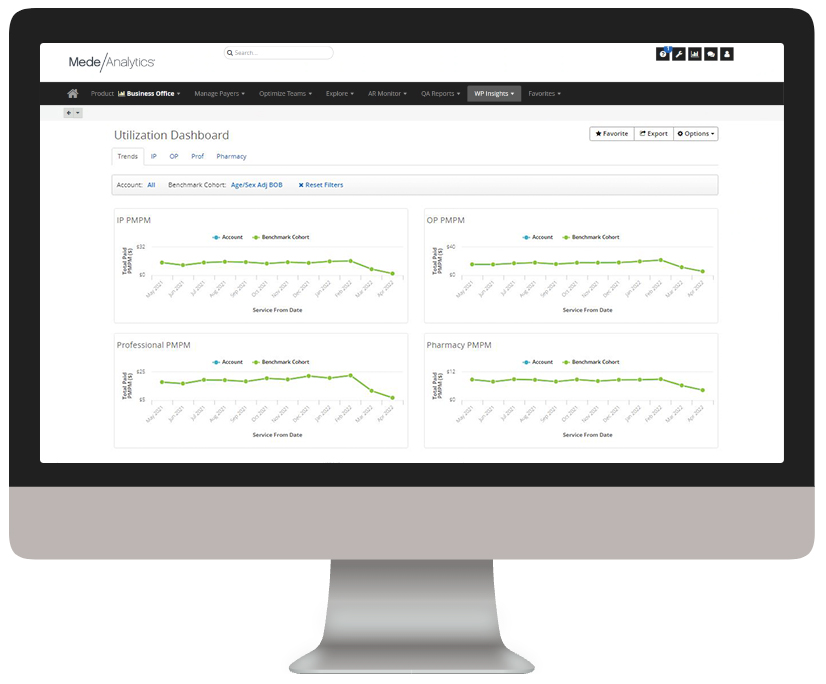
Assess provider quality and member outcomes
Measure and monitor provider performance to identify opportunities for improvements in quality, efficiency and costs
Efficiency, clinical and utilization measures
Explore more on this topic from our experts
10 Strategies for Engaging Providers in Data Dashboards
Payer organizations should be dialed in on data engagement as a key indicator of financial sustainability, successful care delivery, and…
Read on...How did we get here? Hospital analytics and the new normal
I have heard the word “unprecedented” so many times in 2020 that it has lost its significance; many of us have become desensitized to the extraordinary changes in the world this year.
Read on...Bridge the Payer/Provider Data Gap
Every patient has a plethora of data associated with their health record, which can include decades of enrollments, claims, accounts and charges. Much of this data is not housed within the same institutional, facility or provider database…
Read on...Payers and providers: Are you aligned on value-based care?
Value-based care remains top of mind for payers and providers alike. However, continued misalignment between payers and providers can hinder their ability to achieve cost and quality goals. A recent Quest Diagnostics study shows that 62 percent of health plan executives feel that payers have made progress in aligning with providers, while only 41 percent of physicians agree with this notion. What’s more, according to an HFMA survey commissioned by MedeAnalytics, an overwhelming 88% of providers say they are not ready for value-based care.
Read on...