
Did you know that a whopping 30% of the world’s data is healthcare related? 1
Every patient has a plethora of data associated with their health record, which can include decades of enrollments, claims, accounts and charges. Much of this data is not housed within the same institutional, facility or provider database and can be cumbersome and time-consuming to pull together, leaving room for reporting and processing errors. Finding ways to aggregate patient data and maintain it in one place is important because it creates the ability to have immediate, actionable insights, which allows payers and providers to make more informed decisions that save time and money and improve patient outcomes.
Yet, payers and providers traditionally maintain their own slices of patient data, which include enrollment and claims for payers and accounts and charges for providers. Some data elements are unique to payers and some to providers, but much of it overlaps, referencing the same patient events. By rolling up all pertinent claims for an event and connecting to the accounts and charges, payer and provider data can be linked to a single patient event record.
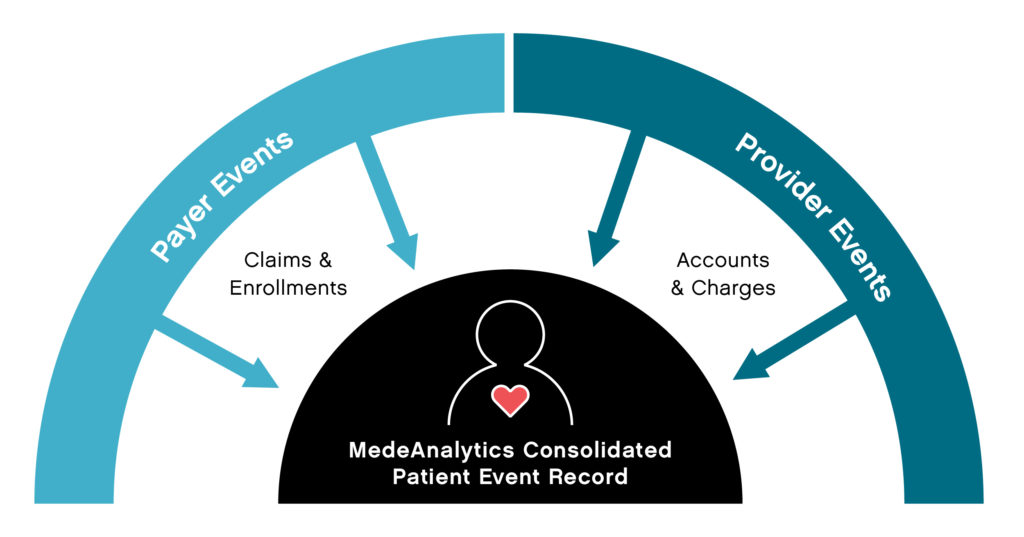
Linking data in this way allows for more collaboration and cohesive information sharing between payers and providers. Providers get access to data that extends beyond the walls of their organization. Payers get much more timely and complete information on their members, bypassing claim lag times. The new data relationship makes available a whole new set of patient-centric reports that were not possible before. Patient event reporting, for example, can provide true insights into mortality, readmissions, hospital-acquired conditions, which are especially critical to ACOs, IDNs and payvider (provider-owned health plans) organizations.
Succinct collection of data and timely dissemination of actionable insights is essential to enable efficient communications between doctors, hospitals, Accountable Care Organizations (ACOs) and health plans. When data is connected, you can accelerate universal speed to insights so that both payers and providers can make smarter decisions, reduce costs, increase organizational efficacy and improve patient outcomes. Learn more.
Get our take on industry trends
Why It’s Time for Healthcare to Move Toward AI Reporting
Business intelligence (BI) was a dramatic and significant step forward in healthcare industry reporting and a natural transition to artificial intelligence (AI) enabled real-time insights.
Read on...Why Healthcare Should “Double-Down” on Exploring AI-powered BI for Reporting
Many areas in healthcare rely not only on the collection of data but, importantly, the ability to decipher and act upon it. In that intersection, reporting was born.
Read on...Why Health Plans and Employers Need Stop Loss Reporting
Due to rising healthcare costs and the Affordable Care Act removing the ban on capitated benefits coverage, numerous employers with self-insured health plans often purchase stop loss coverage. This coverage is not medical insurance; but rather, it’s a financial and risk management tool that protects the employer from excessive claims.
Read on...Bridge the Payer/Provider Data Gap
Every patient has a plethora of data associated with their health record, which can include decades of enrollments, claims, accounts and charges. Much of this data is not housed within the same institutional, facility or provider database…
Read on...


