Value-Based Care Insights
Incentivize partnership in care delivery and patient outcome improvement
As healthcare costs continue to rise and consumers demand greater value, alternative care models are taking on new urgency. For value-based care to be successful, payers, providers and community supports must be engaged and recognize the benefits for themselves and the patients they serve.
To do that well, organizations must ensure that adequate provider networks are in place, providers are measured on quality and cost performance, and reimbursement is based on multiple at-risk and shared savings models to promote higher quality of care at a lower cost. The final key to success is the ability to monitor, analyze, benchmark and improve performance across the ecosystem to exceed value-based care and patient outcome goals.
Comprehensive support for your top value-based care priorities
Value-Based Care Insights enables healthcare payers and providers to improve patient outcomes and satisfaction by delivering higher-quality care at a lower cost. By integrating clinical and claims data, payer and providers gain a 360-degree view into patient/member health that enables actionable insights into population health and risk, provider network performance, and provider quality and measurement.
Program administration
- Program design and definition
- Payment model
- Contract modeling and forecasting
- Contract operations
- Timely reporting
Population health management
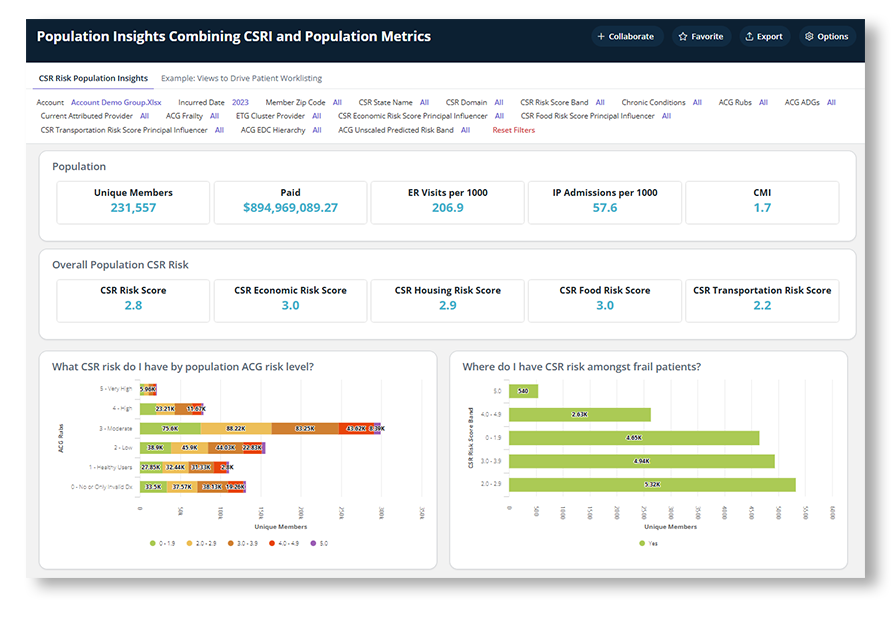
- Risk Adjustment
- Population Attribution
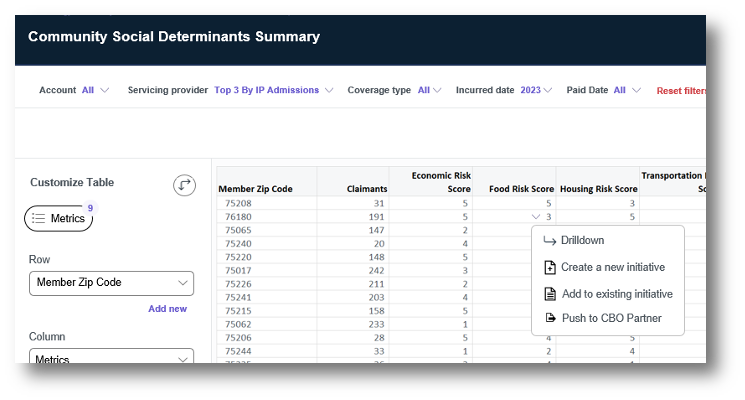
- SDOH / health equity influences
- Care gap identification
- Patient education
Network optimization
- Risk adjustment
- Provider attribution
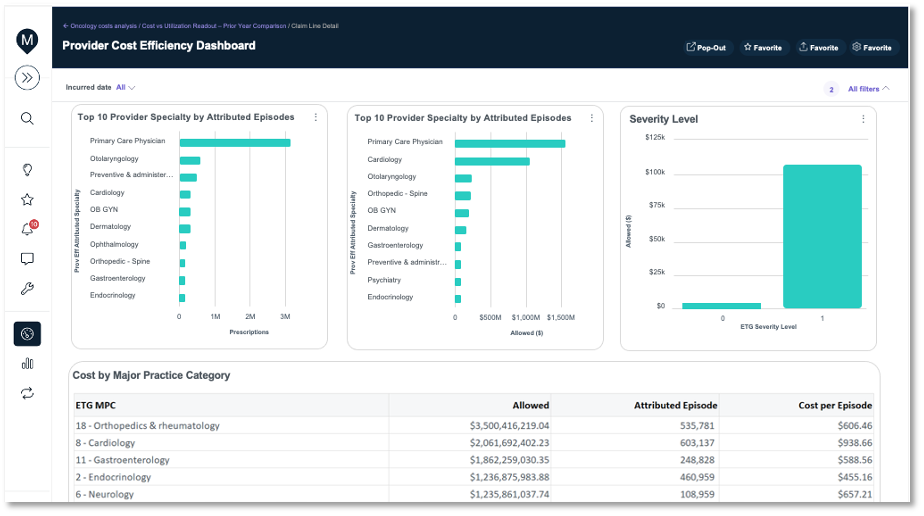
- Provider efficiency
- Network leakage
- Care coordination / transition
Performance reporting
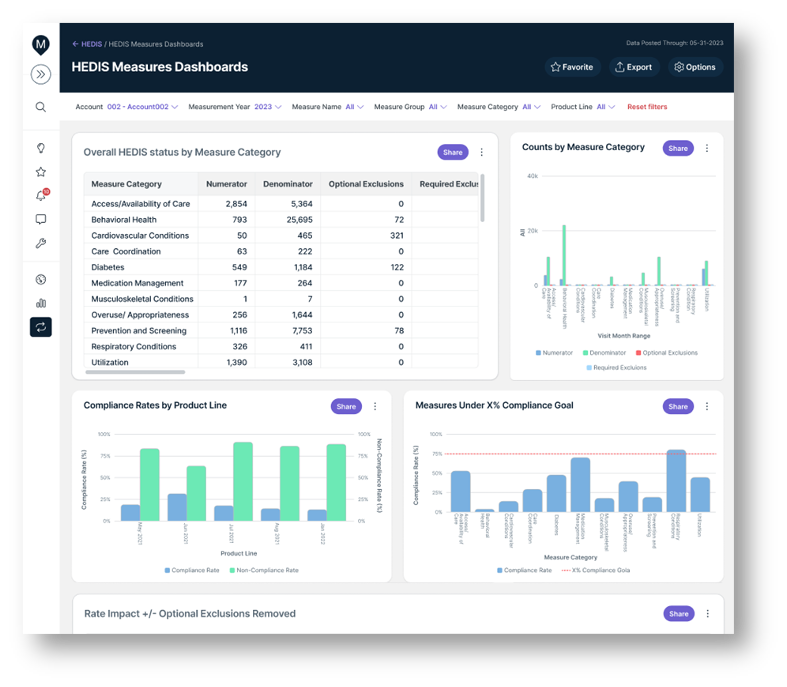
- Clinical measure management
- Provider dashboards
- Cost & utilization metrics
- Patient / member satisfaction
- Financial risk management
Payment & invoicing
- Funding pool management
- Flow of funds management
- Deposit account updates
- Rate & Plan management
- Provider payment reconciliation
Stakeholder engagement
- Provider consent management
- Patient engagement
- Consumer marketing
- Consulting services
- Provider engagement
Augmented analytics
- EMPI / patient matching
- Propensity scoring
- Provider indexing
- Opportunity index
- Forecasting
Data & interoperability
- “Payvider” complexities
- Interoperability
- Integrated dataset management
- EMR Integration
- Unstructured data
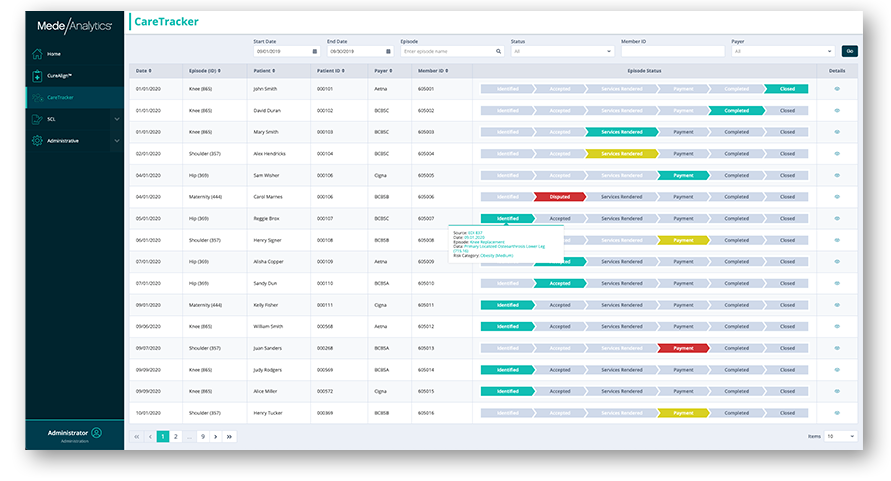
Analytics in action
Our intelligent platform and intuitive user interface make it easy to unlock the value of your data.
In just three clicks, you can access meaningful insights, powerful visualization, and analytics innovation to help you make an even bigger impact.
Dive deeper into Value-Based Care Insights
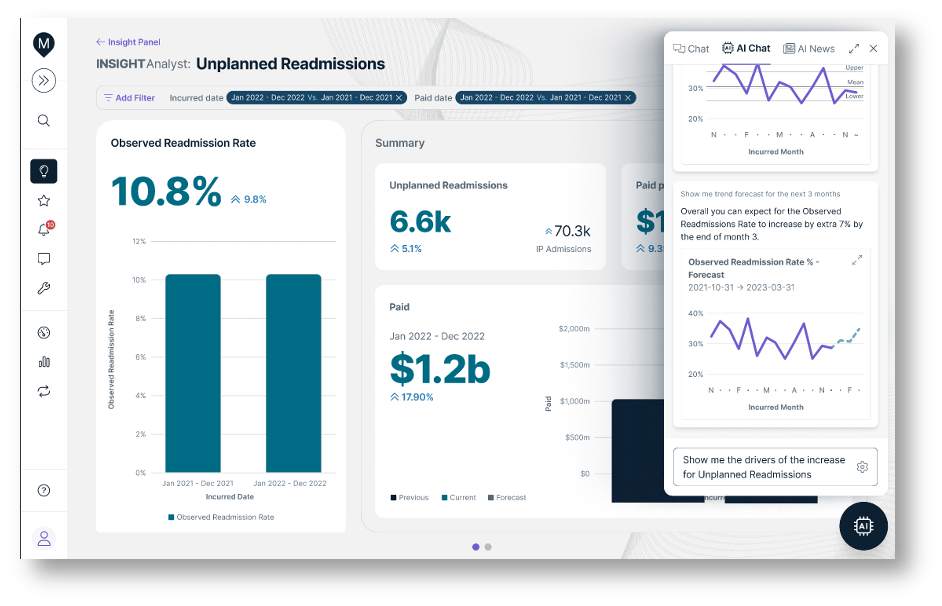
- Artificial Intelligence (AI) tools to rapidly surface key trends
- Seamless connectivity into complementary care management programs to optimize performance
- Participant marketing and activation via multi-modal integrated engagement platform
- Augmented analytics and data science focusing resources on greatest areas of opportunity
- Provider onboarding automated and at scale
Leading organizations; exceptional accomplishments
Visit our Value-Based Care Blueprint page for everything you need to know to navigate the intersection of value and analytics.
Get our take on industry trends
Run: Bringing Data Science into your Organization
In this three-part series, we’ve been detailing a tiered approach to introducing and incorporating data science into your organization. In Part One: Crawl and Part Two: Walk, we discussed how to get started from scratch and start building out a dedicated data science program. Today, we’ll dive into the third and final phase to see how to grow quality, centralize governance, incorporate user feedback, and more.
Read on...Walk: Bringing Data Science into your Organization
In this three-part series, we’re exploring a tiered approach to introducing and incorporating data science into your organization. In Part One: Crawl, we discussed how to get started from scratch. Today in Part Two: Walk, we’ll address issues that may emerge and how to overcome them, how to build out a dedicated data science team, and more.
Read on...Crawl: Bringing Data Science into your Organization
Throughout my career as a data scientist, I’ve been lucky enough to have a few opportunities to build data science…
Read on...Tell the best healthcare story with data dashboards
By this point, we’ve all heard the statistic that healthcare data is growing at 36% annually. The result of this…
Read on...Want to talk with one of our experts?
We're driving data-powered improvement across the industry

Healthcare payers and health plans
Healthcare Payers and health plans
deploy our value-based care and provider network analytics to enhance population health, quality and network management and empower their employers and brokers through self-service analytics.

Healthcare providers and health systems
Healthcare Providers and Health Systems
use our end-to-end revenue cycle management analytics to lower denials, accelerate A/R, and improve staff productivity.

Government Medicare and Medicaid programs
Government Medicare and Medicaid programs rely on our comprehensive dashboards to understand cost drivers, gaps in care, and social determinants impacting beneficiary outcomes.