Workforce Quality Insights
End-to-end insights to improve financial health
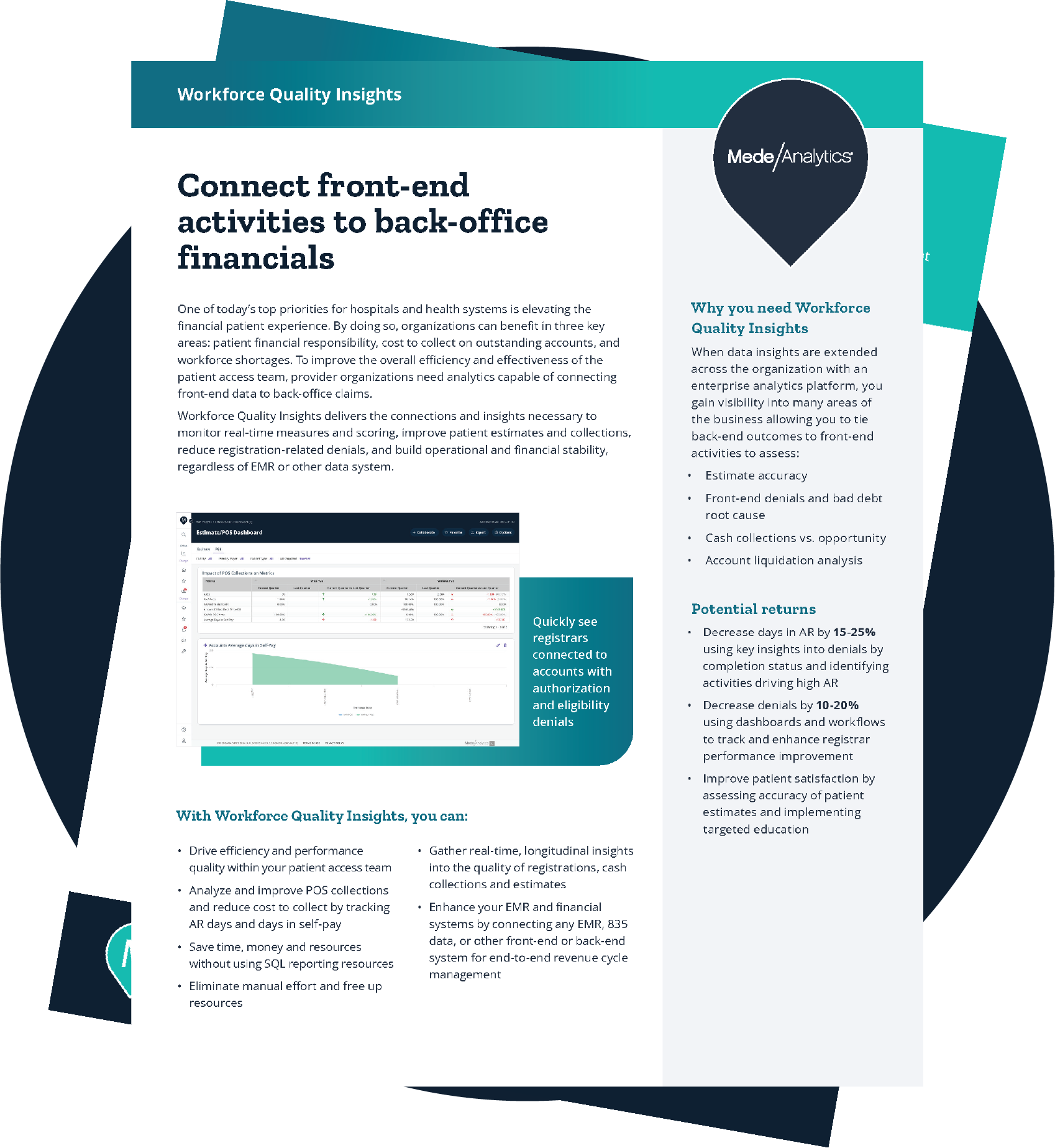
Traditional approaches to revenue cycle optimization slice up the process into distinct parts and platforms and attempt to solve each challenge in a vacuum. With denials, cost-to-collect, self-pay AR, and patient financial responsibility all increasing, you can no longer afford to make important decisions based on fragmented operations and disconnected data (literally).
Our Workforce Quality Insights breaks down these barriers, using powerful analytics capabilities to generate end-to-end insights into how patient access activities are impacting back-office outcomes.
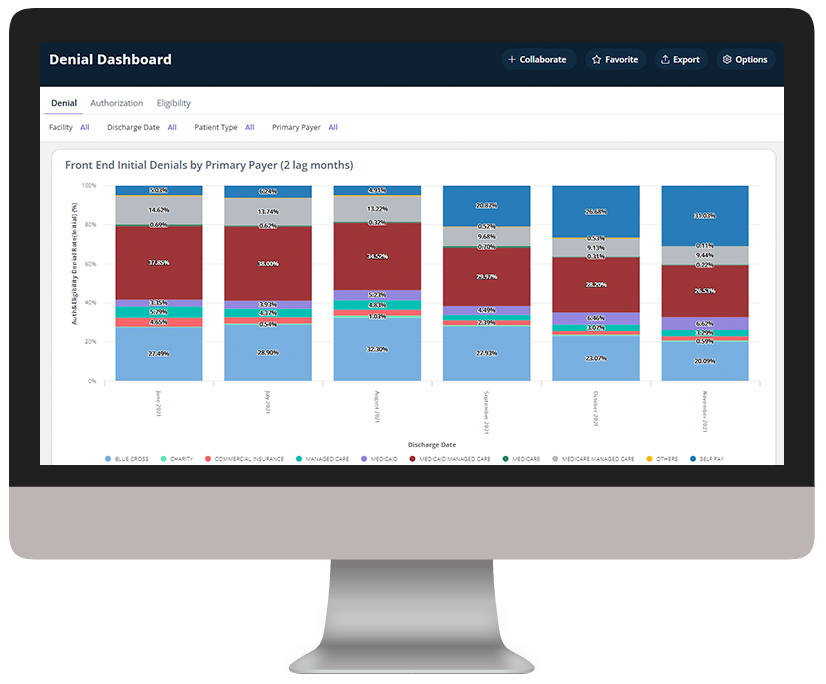
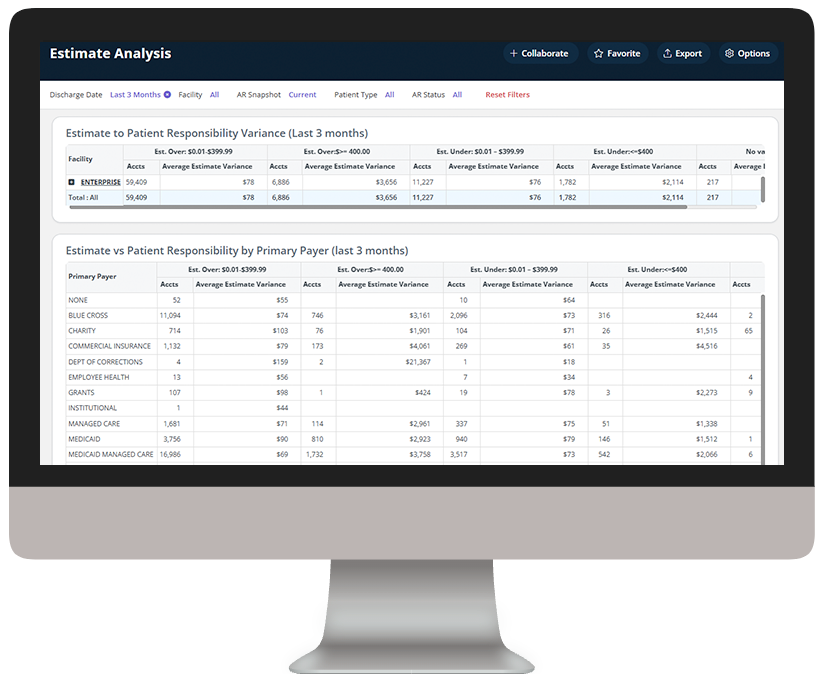
Connecting front-end data to financial outcomes
Challenge
Solution
Bridging upstream activities and downstream financial outcomes requires significant manual effort and can’t get to the level of detail needed to focus staff process improvements.
Challenge
Solution
Errors and inefficiencies are magnified and multiplied as they go unchecked throughout the revenue cycle.
Challenge
Solution
Remote staff use disjointed systems, making it difficult to determine the effect of registrar activities on revenue cycle outcomes.
Challenge
Solution
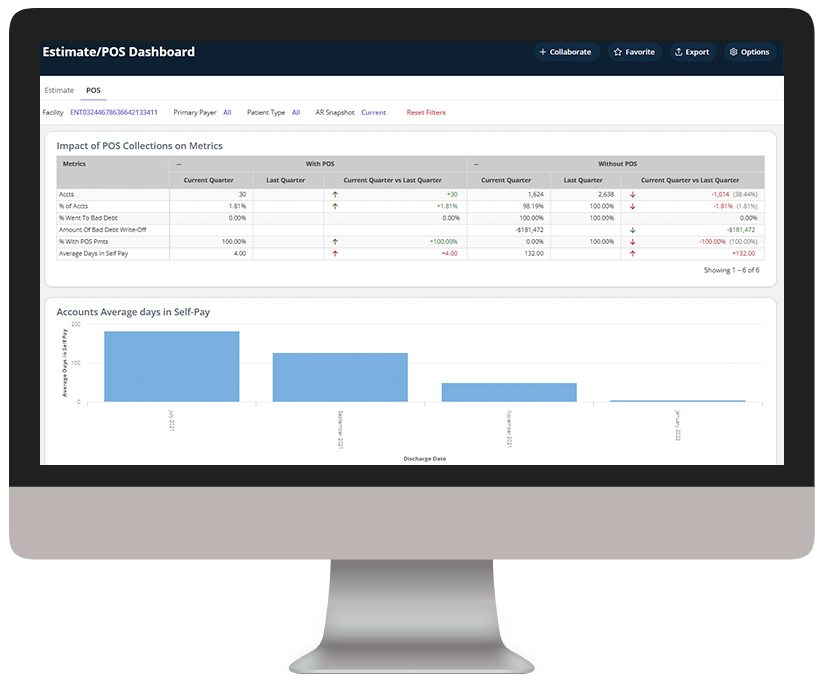
Siloed data and poor front-end performance causes increased denials, inaccurate estimates, and improper POS collections leading to higher days in AR and days in self-pay.
You could achieve...
Analytics in action
Workforce Quality Insights can be used with any combination of MedeAnalytics solutions, third party analytics, or EHR system to make the necessary data linkages that facilitate end-to-end revenue cycle performance improvement. In as little as three clicks, you can access meaningful insights, powerful visualization, and analytics innovation to help you make a bigger impact on performance.
Explore a few key features by hovering over the image.
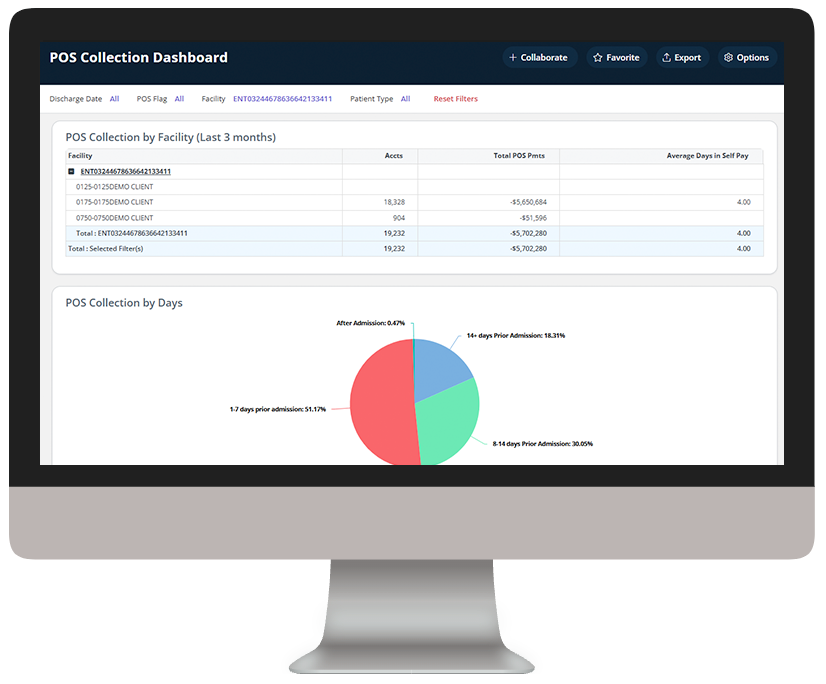
Examine POS collections to prioritize efforts
Dive deeper into Workforce Quality Insights
Download the data sheet for next-level details about how Workforce Quality Insights can transform your organization’s financial health.
Get our take on industry trends
You’re asking too much of your EHR
Electronic Health Records (EHRs) are purported to do a lot of things to support healthcare providers, and most of their claims are generally accurate. Of course, like anything, there are many areas where EHR vendors could and should make improvements.
Read on...Gamification in healthcare only works if you can measure it – here’s how
In business and in sports, it’s all about teams. What teams can accomplish when they work together. How they can fail spectacularly when they do
Read on...Pandemic fuels 2021 healthcare megatrends
When I wrote about megatrends last year, the predictions were, naturally, forward-looking. Telehealth, for example, was important because of increased healthcare consumerism and the convergence of technologies to make its use quick and easy for payers, providers and patients.
Read on...Measuring provider cost and utilization
No matter the time of year, payers and providers should work to agree on a shared source of truth when it comes to data. With the recent end of the year, it’s time to celebrate the new year (who isn’t ready to say goodbye to 2020?) and close the books, which includes the reconciliation of any shared savings or losses.
Read on...Want to talk with one of our experts?
Provider Value Analytics: Our full lineup of provider solutions
Everything you need to support your front office, mid-cycle and back office.
Patient
Access
Insights
Optimize patient satisfaction during the patient registration and payment clearance processes with critical, real-time analytics information.
Revenue Integrity
Suite
See how clinical operations affect your bottom line with complete visibility into compliance risk and clinical documentation performance.
Business Office
Suite
Achieve optimized cash flow and operational excellence with big-picture insight into opportunities for improving collection rate, denials, and staff productivity.

Workforce Quality Insights
Use powerful analytics capabilities to generate end-to-end insights into how patient access activities are impacting the back-office outcomes.
Cost
Insights
Drill down into claims and encounter-level data to target and align controllable costs with outcomes and reimbursement.
Productivity
Analytics
Collect and deliver real-time insights on individual and collective registrar performance, and identify opportunities for training.