Quality Insights
Improve value-based care quality and population health outcomes
The rise of value-based care has inevitably spurred heightened focus on quality improvement across the healthcare ecosystem. There are two sides to this coin: measures and members. On the measures side, health plans are working to align with strict national standards and state-specific requirements (think: HEDIS, Star ratings). On the members side, payers are striving to understand their patient populations more fully and provide more timely, appropriate interventions.
Delivering comprehensive solutions to enhance performance and outcomes
Challenge
Solution
Siloed, incompatible information from EMRs, claims and other sources hinder efficient quality calculations and data submission
Challenge
Solution
Unnecessary ED visits and readmissions drive up costs and decrease member satisfaction
Challenge
Solution
Insufficient, unreliable data on clinical performance deters provider engagement
Celebrating big wins with Quality Insights
Analytics in action
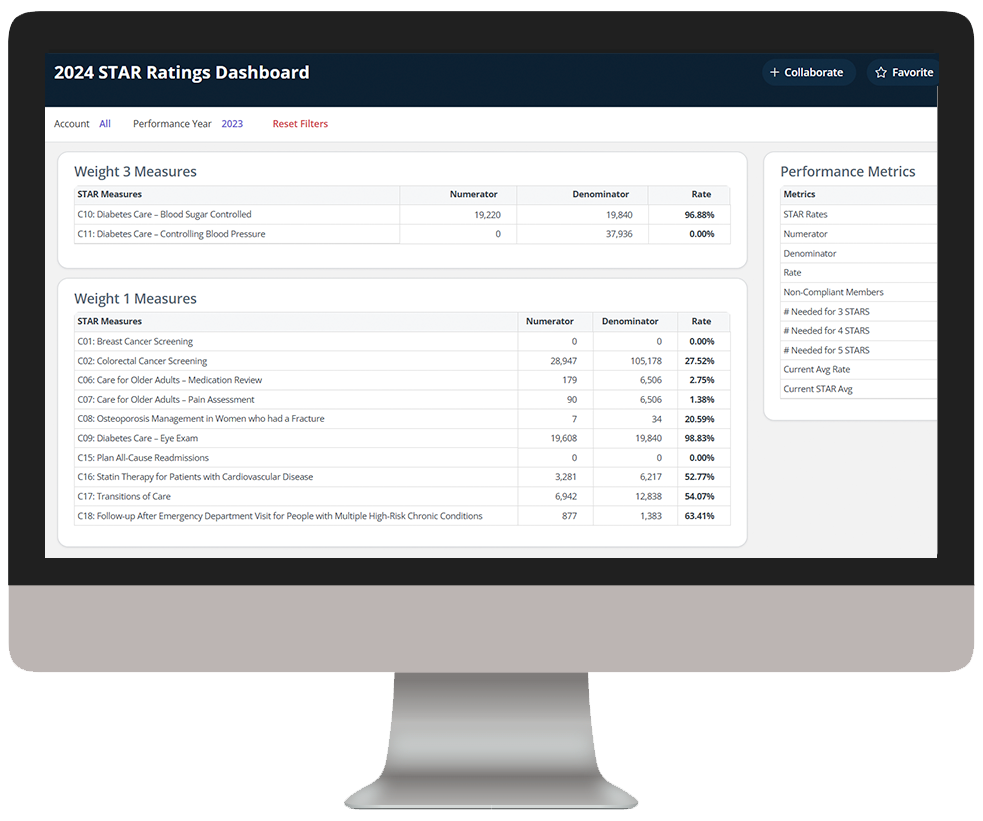
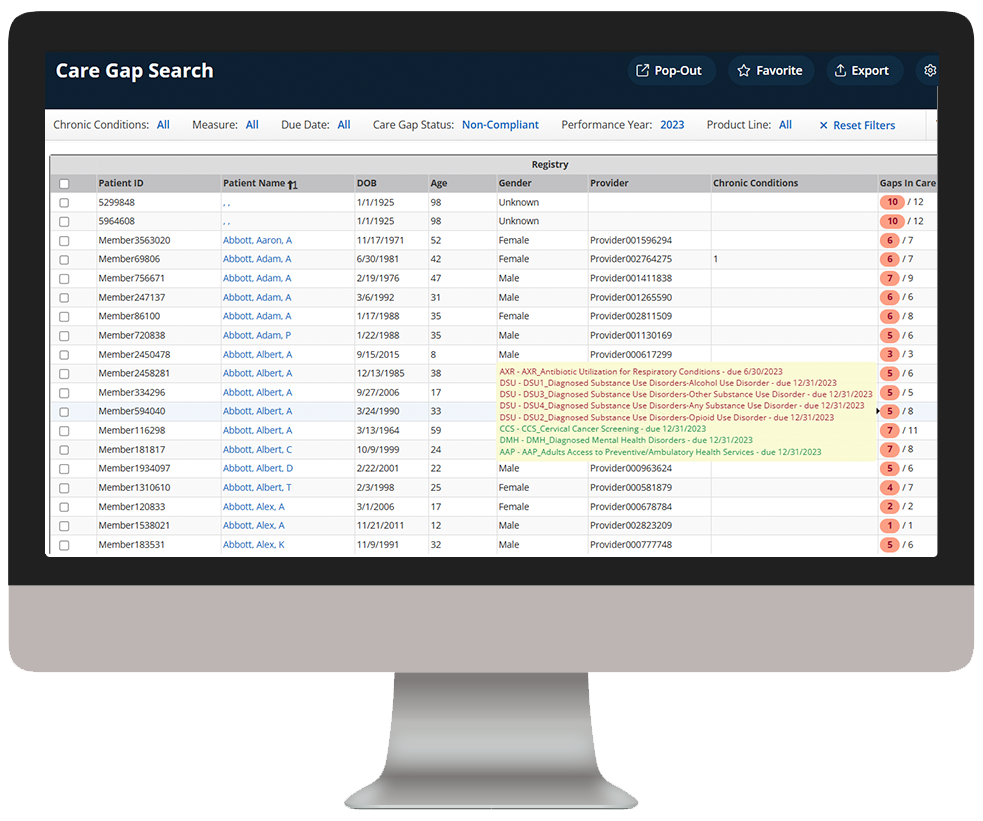
Our intelligent platform and intuitive user interface make it easy to unlock the value of your data. In as little as three clicks, we bring meaningful insights, powerful visualization, and analytics innovation to help you make an even bigger impact at your organization.
As you click through our example dashboards, hover over the image to explore a few key features.
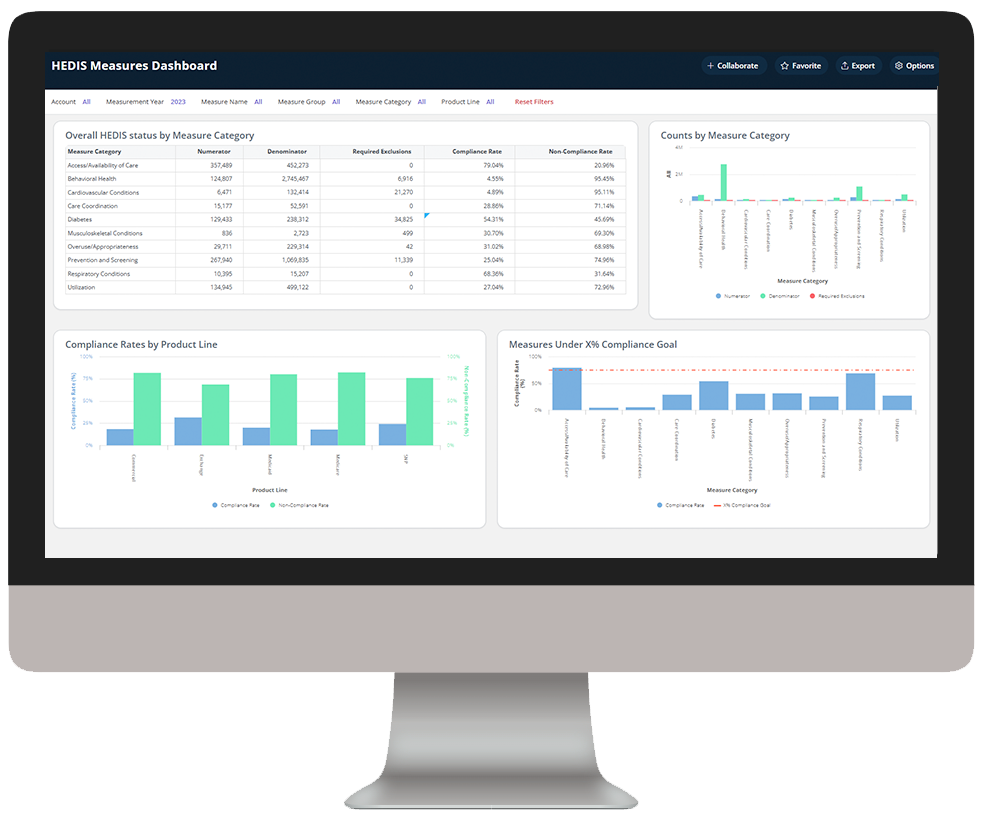
Assess HEDIS measure performance and compliance
Dive deeper into Quality Insights
Download the data sheet to see how Quality Insights can help your health plan improve care quality and outcomes.
Visit our Value-Based Care Blueprint page for everything you need to know to navigate the intersection of value and analytics.
Get our take on industry trends
Why Healthcare Should “Double-Down” on Exploring AI-powered BI for Reporting
Many areas in healthcare rely not only on the collection of data but, importantly, the ability to decipher and act upon it. In that intersection, reporting was born.
Read on...Why Health Plans and Employers Need Stop Loss Reporting
Due to rising healthcare costs and the Affordable Care Act removing the ban on capitated benefits coverage, numerous employers with self-insured health plans often purchase stop loss coverage. This coverage is not medical insurance; but rather, it’s a financial and risk management tool that protects the employer from excessive claims.
Read on...Bridge the Payer/Provider Data Gap
Every patient has a plethora of data associated with their health record, which can include decades of enrollments, claims, accounts and charges. Much of this data is not housed within the same institutional, facility or provider database…
Read on...Digging deeper: Leveraging analytics to boost service line profitability
Regardless of the size of the hospital or health system, you need to look beyond traditional operational metrics to fully understand your organization’s performance. Insights into revenue, volume, cost, quality and variation across service lines are key to improving both performance and profitability.
Read on...Want to talk with one of our experts?
Payer Value Analytics: Our full lineup of payer solutions
Everything you need to step into the future of healthcare and drive real change across populations.
Quality Insights
Activate insights into population health and quality to improve satisfaction and outcomes for members and maintain a competitive position in the market.
Employer Insights
Elevate data sharing with employer groups to demonstrate plan value and increase efficacy of risk stratification and care management plans.
Network Insights
Accelerate provider performance with evidence-based outcomes comparisons, cost-effectiveness analyses, and extensive segmentation capabilities.