The healthcare financial landscape is constantly in a state of flux— with ICD-10, fee-for-value reimbursement, and shared accountability payment models contributing to the significant change – but one thing remains the same: uncompensated care is at an all-time high. To help providers navigate their financial health, MedeAnalytics Business Office provides insight into revenue and cost savings opportunities, by bringing complex patient accounting data into a unified view.
Comprised of several financial management tools our Revenue Cycle and Business Office solutions offer data analysis on accounts receivable, denials, bad debt, and payer contracts. Here are the top three tips and tricks you might consider when using the solution:
#1: Think Payer Management, not Payer Monitoring
Mitigate wasted staff time due to delay tactics and confusing information from payers. Intelligent insights allow you to manage and compare behavior on a payer-by-payer basis in order to optimize team efficiency.
#2: Shift Your Focus from Denial Appeals to Denial Prevention
Denial rates have increased in the past two years and appeal success rates for most organizations are falling short. You can get ahead of this by reallocating appeal resources towards prevention and focusing on avoidable errors based on historical results and trends.
#3: Smarter, not Harder, Self-Pay Collections
Due to the larger number of high-deductible ACA plans, the patient is now becoming one of, if not the largest payer. Streamline self-pay collections efforts by using predictive models to compute a patient’s propensity to pay.
Not using Business Office, but curious to learn more? Check out the Business Office solution page to read about the benefits.
Get our take on industry trends
Best practice tools to build an integrated approach to multimorbidity
The traditional model of treating single diseases no longer works. Data collected from 2016 to 2019 indicated that 32.9% of…
Read on...Will adopting a risk-based approach with augmented analytics support care gap closure?
A common challenge for healthcare systems is how to properly segment its patient populations based on risk profiles and co-morbidities. Doing this well ensures a high quality of care delivery and superior patient outcomes.
Read on...4 questions healthcare executives are asking about augmented analytics
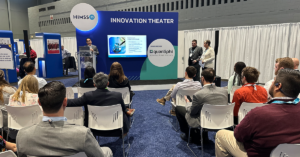
At our annual Impact Summit, I had the privilege to talk about augmented analytics and address questions from healthcare executives—many…
Read on...