The healthcare reimbursement landscape is continuously changing, creating numerous challenges for healthcare organizations as they look to increase revenue. In fact, the revenue risk among not-for-profit and rural healthcare systems are even greater. The National Rural Hospital Association, estimated that 673 rural facilities were at risk of closure, out of over 2,000. West Tennessee Healthcare (West Tennessee), one of the largest, rural, public, not-for-profit healthcare systems in the U.S, acted proactively to combat this trend. In our recent case study, we examine how West Tennessee leveraged analytics to achieve financial success.
West Tennessee has four hospitals, two medical centers and offers 20 primary and specialty care centers. They service a population of 500,000 and with such a large rural patient base, needed guidance to address the following issues:
- 3:1 bad debt to charity ratio
- High percentage of accounts in arrears
- Long lead (30+ days) to denial and appeal process
West Tennessee’s Executive Director of Patient Financial services, Wade Wright, noted that with our help they improved upon the following areas, including:
- Denials workflow and triage – A centralized, efficient denial management approach, allowed them to quickly address denials and overturn accounts.
- Self-pay Analytics – The implementation of a presumptive charity program reduced their bad debt to charity ratio.
- Smart work lists – By creating targeted lists, they could drive efficient workflows and prioritize and segment accounts.
- Self-service data analytics – Meaningful and easy-to-use data tools gave them the ability to shine a spotlight on pain points and obtain the biggest return on investment.
By integrating Patient Access and Revenue Integrity, along with Business Office, West Tennessee had an end-to-end revenue cycle management solution. This helped them to reduce their bad debt to charity ratio to 1:1 and the percentage of accounts in arrears by 3.3 percent. Their billed accounts receivable also dropped by $34.9 million in only four months. By applying our analytics solutions, West Tennessee successfully overcame their revenue cycle management barriers and are better prepared for future healthcare changes.
To read more about our partnership with West Tennessee, click here. You can also download our infographic here. If you’re interested in learning how you can achieve similar results within your organization, request a demo with us: https://medeanalytics.com/request-demo
Get our take on industry trends
Best practice tools to build an integrated approach to multimorbidity
The traditional model of treating single diseases no longer works. Data collected from 2016 to 2019 indicated that 32.9% of…
Read on...Will adopting a risk-based approach with augmented analytics support care gap closure?
A common challenge for healthcare systems is how to properly segment its patient populations based on risk profiles and co-morbidities. Doing this well ensures a high quality of care delivery and superior patient outcomes.
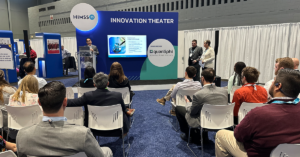
Read on...4 questions healthcare executives are asking about augmented analytics
At our annual Impact Summit, I had the privilege to talk about augmented analytics and address questions from healthcare executives—many…
Read on...