Insights
Featured:
Enhancing healthcare delivery with explainable AI: A methodological leap forward
By Matthew Hanauer, Ph.D.
Articles
Enhancing healthcare delivery with explainable AI: A methodological leap forward
Healthcare providers and payers continually seek methods to enhance patient care and operational efficiency. With the advent of complex data…
Another year, another great HIMSS!
HIMSS24 was a fantastic event, as always. One of our favorite additions this year was the Digital Health Technology Theme…
Optimize your midcycle for telehealth services
Telemedicine is now a permanent fixture in homes across America. A majority of healthcare organizations have established the technology necessary…
Blueprints
Augmented
analytics
Explore what augmented analytics is, the benefits it can bring to healthcare, and tips for leveraging it.
Value-based
care
Check out our resources for how to find success at the intersection of analytics and value.
Go to the Value-based Care Blueprint
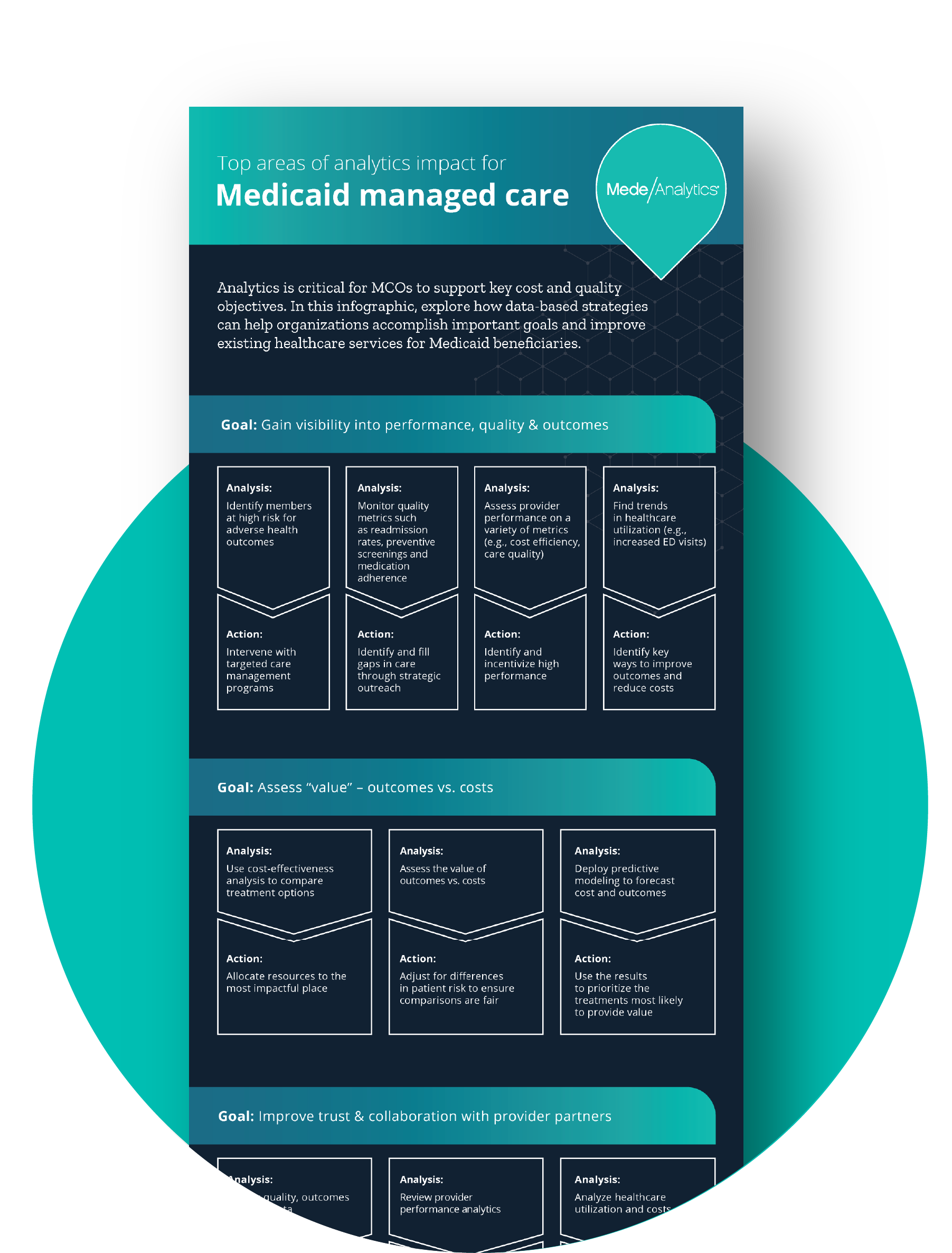
Medicaid &
managed care
Education, direction, and inspiration to support your care access, equity, and delivery goals.
Go to the Medicaid & Managed Care Blueprint
Featured infographic
Analytics is critical for MCOs to support key cost and quality objectives.
Download this resource to explore how data-based strategies can help organizations accomplish important goals and improve existing healthcare services for Medicaid beneficiaries.
Press release
MedeAnalytics and Socially Determined partner to provide a more holistic view of patients and members with integrated social determinants of health data
This pivotal partnership paves the way for optimized value-based care through actionable SDOH insights. MedeAnalytics CEO Steve Grieco spoke to the immense benefits stating, "This will allow further risk stratification for focused interventions, leading to better care coordination, patient engagement, cost savings, and stronger, healthier communities."