Blueprint:
Education, direction, and inspiration to support your care access, equity, and delivery goals
The COVID-19 pandemic and its economic impact have had significant implications for Medicaid spending and enrollment. After a two-year decline, Medicaid enrollment rose 25.6% and saw a sharp spending increase totaling over $728 B in FY 2021.
However, even with a steep increase in its use, emergency regulations and coverages put in place during the pandemic are unwinding and ending (see this early example from Arkansas). Medicaid programs are feeling the hit of these changes; the Kaiser Family Foundation estimates between 5.3 and 14.2 million Medicaid users could be disenrolled. Within that, nearly 7 million are projected to lose Medicaid coverage despite being eligible due to logistical, procedural and administrative barriers that disproportionately affect people of color. States have just 14 months (May 2023 through September 2024) to determine how to proceed and return to ‘normal’ operations.
Payers are also grappling with care access and affordability challenges brought on by healthcare worker shortages, price inflation, and aggressive consolidation in the market.
States must meet numerous requirements within their Medicaid programs to receive federal funding—one of which is utilizing managed care. Consequently, MCOs are the dominant delivery system for Medicaid enrollees with 72% of Medicaid beneficiaries enrolled nationally. Over time, laws have shifted to both add flexibility for states’ use of managed care and ensure a direct chain of accountability from Congress to states and states to MCOs.
Managed care plans vary significantly, as each state has the power to decide:
- Which populations and services to include in managed care arrangements
- How much MCOs are paid per member per month
- What mechanisms are deployed to adjust plan risk, incentivize plan performance, and ensure payments are not too high or too low
In turn, MCOs must initiate strategies to meet their own goals, including:
- Controlling patient access to specialized care
- Eliminating unnecessary services
- Integrating health care delivery and payment systems through prepaid member fees
- Limiting provider fees by establishing fixed rates for physicians and hospital services
- Controlling drug costs by implementing pharmacy benefits management plans
The big challenge: How can MCOs remain accountable to the states while providing the best care to their beneficiaries?
Successful MCOs are utilizing data to address cost issues, achieve quality requirements, and facilitate decision-making. Data must be complete, accessible and actionable in an easy-to-use analytics platform that can take plans from objectives to successes.
Analytics equips MCOs to combine quality, cost, utilization management, SDOH, enrollment and eligibility data into a 360-degree member view. It also generates insights to help health plans devise new—and improve existing—healthcare services for Medicaid beneficiaries.
Below are examples of how analytics can support success in several key areas.
MCOs play a critical role in improving population health through various interventions, programs and initiatives aimed at identifying and reducing gaps in care.
- Identify high-risk populations: Use analytics tools to identify individuals with chronic conditions or those with multiple hospitalizations to target interventions aimed at improving health outcomes and reducing costs.
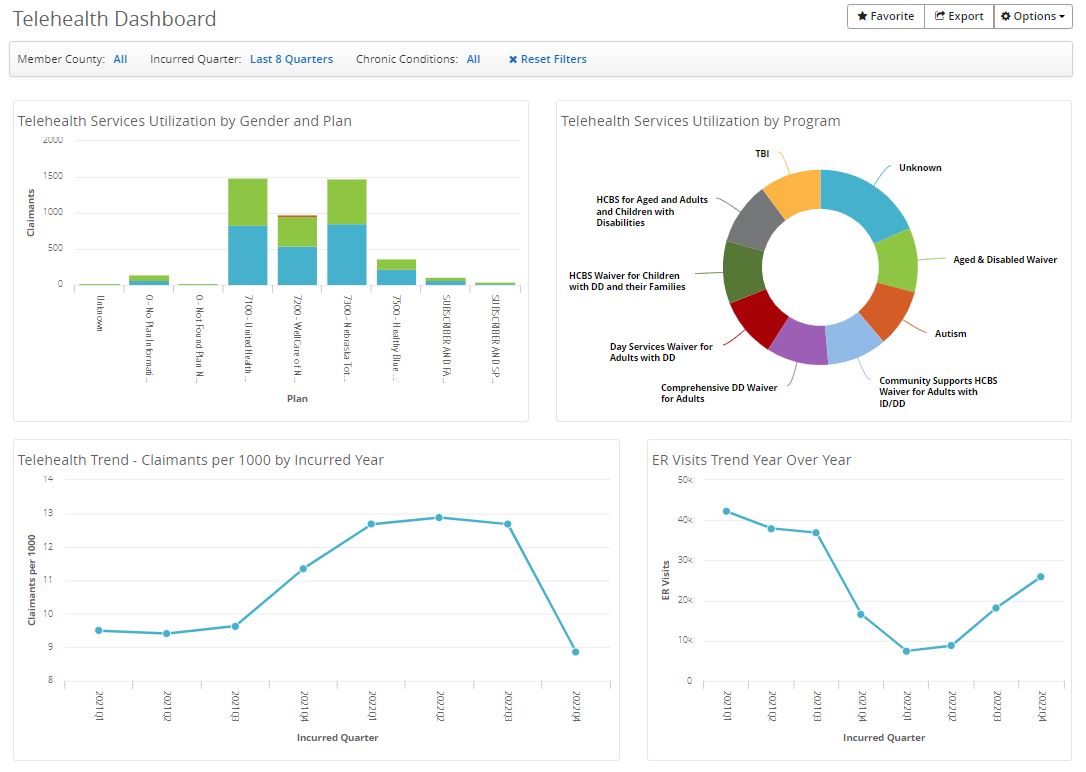
- Manage member utilization: Monitor utilization to ensure members are receiving appropriate care and services. Reduce unnecessary or inappropriate healthcare services to improve health outcomes and reduce costs.
- Improve disease management: Develop data-driven programs that focus on preventive care and early intervention for chronic conditions such as diabetes, heart disease and asthma.
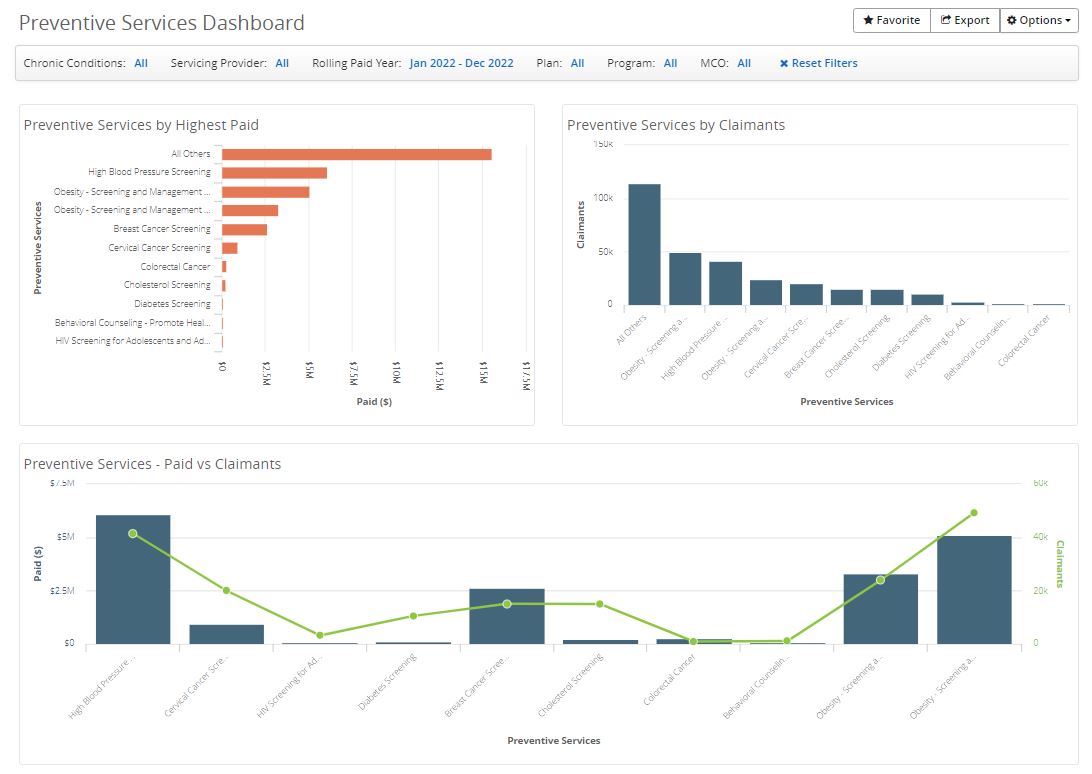
- Set up wellness and prevention programs: Use claims and clinical data to identify areas of opportunity for wellness programs that include health screenings, smoking cessation, weight management and fitness classes.
- Advance care coordination: Consolidate care management resources across the care continuum to ensure members receive coordinated and comprehensive care without duplicating services.
Don’t miss invaluable insights into the most impactful payer challenges and opportunities of our day
Position your organization for success under CMS-HCC V28
The transition from CMS-HCC V24 to V28 heralds a significant shift in risk adjustment methodologies and emphasizes improved accuracy and…
Read on...Best practice tools to build an integrated approach to multimorbidity
The traditional model of treating single diseases no longer works. Data collected from 2016 to 2019 indicated that 32.9% of…
Read on...Using data analytics to combat the maternal health crisis
With most pregnancy-related deaths being considered preventable, why is the United States facing a maternal health crisis? The country’s maternal mortality rate is the highest of any developed nation in the world and more than double the rate of peer countries.
Read on...