Workforce Performance Insights
Connecting data to cultivate financial health
Provider organizations house large quantities of data on front-end patient interactions. When applied correctly, that information can be leveraged to understand payment outcomes, correlate encouraged actions to financial gains, and identify training opportunities for revenue cycle management teams. Unfortunately, most information systems are not equipped to execute this type of analysis. With MedeAnalytics Workforce Performance Insights, we are connecting critical registrar and patient access information with back-office financial data to improve team efficiency and cultivate financial health.
Part of the Workforce Quality Insights suite:
Aligning registrar performance to patient experience goals
Challenge
Solution
Incorrect estimates for non-emergent care lead to outstanding accounts receivable and time-consuming follow up
Challenge
Solution
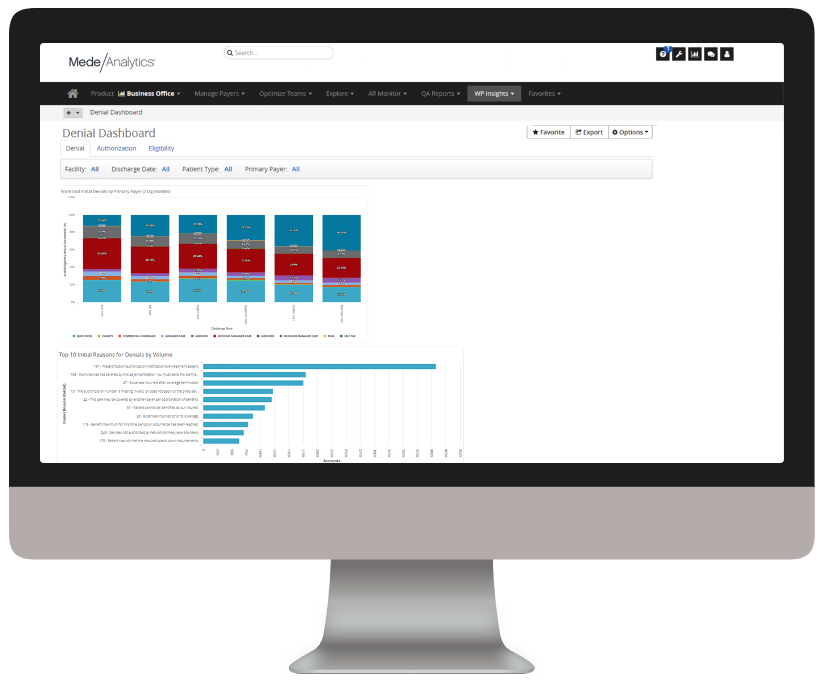
Lack of specificity in denials reporting results in repeated mistakes and decrease in trust
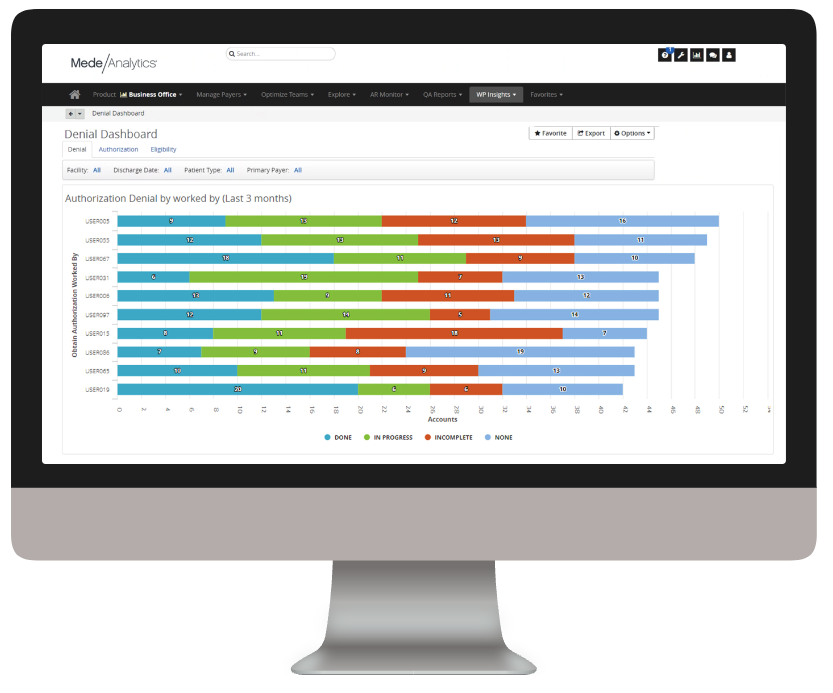
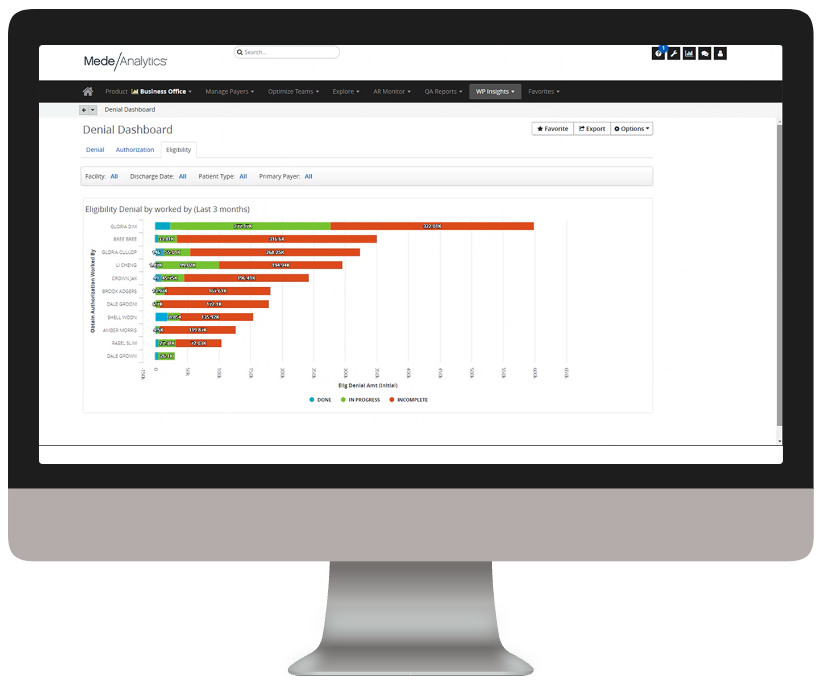
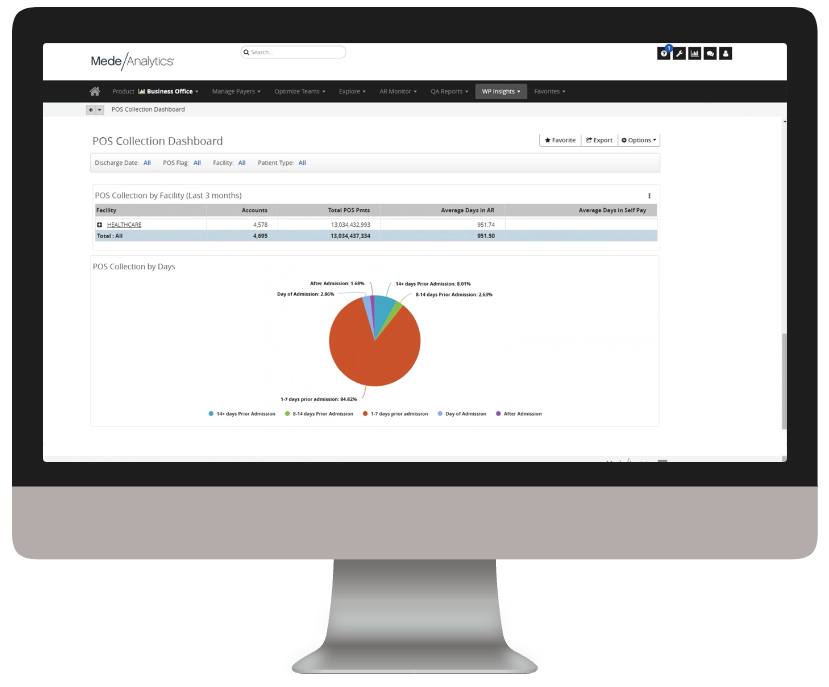
Analytics in action
Our intelligent platform and intuitive user interface make it easy to unlock the value of your data. In as little as three clicks, we bring meaningful insights, powerful visualization, and analytics innovation to help you make an even bigger impact at your organization.
Explore a few key features by hovering over the image.
Quickly toggle between dashboards on Collections, Denials, Estimate Accuracy and personalized reports
See when and where you are having success with POS collections to create best practices and determine where you can make improvements
Export results to others or for use in presentations to quickly show how pre-service activities are affecting financial results
Dive deeper into Workforce Performance Insights
Download the data sheet to see how Workforce Performance Insights helps you connect workflow activities and financial outcomes to protect patient financial experience and ensure organizational stability.
Get our take on industry trends
Introduction to social risk: What healthcare leaders need to understand
‘Social determinants of health’ has been a common phrase for decades now, but the term social risk is much less…
Read on...AI is your new crystal ball: How predictive analytics can reduce denials
The idea of having a crystal ball to better understand what claims will be denied is an awesome concept. But one we can’t rely on. Thankfully, we have predictive analytics to take the place of a crystal ball.
Read on...3 ways to reduce friction in payer-provider relationships
The dynamic between healthcare providers and payers has historically been quite strained. Though both parties are interested in improving the…
Read on...Position your organization for success under CMS-HCC V28
The transition from CMS-HCC V24 to V28 heralds a significant shift in risk adjustment methodologies and emphasizes improved accuracy and…
Read on...Want to talk with one of our experts?
Provider Value Analytics: Our full lineup of provider solutions
Everything you need to support your front office, mid-cycle and back office.
Patient
Access
Insights
Optimize patient satisfaction during the patient registration and payment clearance processes with critical, real-time analytics information.
Revenue Integrity
Suite
See how clinical operations affect your bottom line with complete visibility into compliance risk and clinical documentation performance.
Business Office
Suite
Achieve optimized cash flow and operational excellence with big-picture insight into opportunities for improving collection rate, denials, and staff productivity.

Workforce Quality Insights
Use powerful analytics capabilities to generate end-to-end insights into how patient access activities are impacting the back-office outcomes.
See the solution ❯
Cost
Insights
Drill down into claims and encounter-level data to target and align controllable costs with outcomes and reimbursement.