
Compliance+
Amid a slew of compliance requirements, daily problems to solve, and overarching organizational goals, it can be difficult for provider organizations to organize improvement efforts and dedicate resources appropriately. Compliance+ is a complete workflow and analytics solution for compliance teams that need to proactively assess their at-risk claims, gain insights into ways to decrease mid-cycle denials, and show how their impact is affecting A/R trends.
Part of the Revenue Integrity Suite:
Connect compliance improvements to financial success and sustainability
Challenge
Solution
Basic reporting limits compliance team’s advancement
Challenge
Solution
Isolated data sets prevent benchmarking and comparisons
Analytics in action
Our intelligent platform and intuitive user interface make it easy to unlock the value of your data. In as little as three clicks, we bring meaningful insights, powerful visualization, and analytics innovation to help you make an even bigger impact at your organization.
Explore a few key features by hovering over the image.
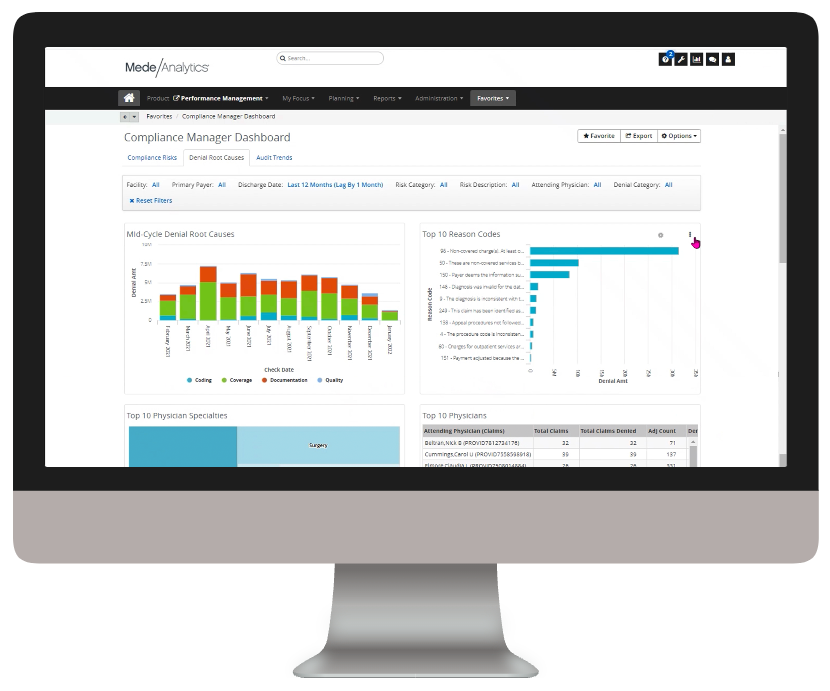
Gain insights into your at-risk claims, coding and documentation denials, and audit trends from a single dashboard
Quickly export reports and share insights on denial and audit trends
Filters allow for slicing and dicing without leaving your overview dashboard
Dive deeper into Compliance+
Download the data sheet to learn more about how Compliance+ saves hours in reporting.
Get our take on industry trends
You’re asking too much of your EHR
Electronic Health Records (EHRs) are purported to do a lot of things to support healthcare providers, and most of their claims are generally accurate. Of course, like anything, there are many areas where EHR vendors could and should make improvements.
Read on...Gamification in healthcare only works if you can measure it – here’s how
In business and in sports, it’s all about teams. What teams can accomplish when they work together. How they can fail spectacularly when they do
Read on...Pandemic fuels 2021 healthcare megatrends
When I wrote about megatrends last year, the predictions were, naturally, forward-looking. Telehealth, for example, was important because of increased healthcare consumerism and the convergence of technologies to make its use quick and easy for payers, providers and patients.
Read on...Measuring provider cost and utilization
No matter the time of year, payers and providers should work to agree on a shared source of truth when it comes to data. With the recent end of the year, it’s time to celebrate the new year (who isn’t ready to say goodbye to 2020?) and close the books, which includes the reconciliation of any shared savings or losses.
Read on...Want to talk with one of our experts?
Provider Value Analytics: Our full lineup of provider solutions
Everything you need to support your front office, mid-cycle and back office.
Patient
Access
Insights
Optimize patient satisfaction during the patient registration and payment clearance processes with critical, real-time analytics information.
Revenue Integrity
Suite
See how clinical operations affect your bottom line with complete visibility into compliance risk and clinical documentation performance.
Business Office
Suite
Achieve optimized cash flow and operational excellence with big-picture insight into opportunities for improving collection rate, denials, and staff productivity.

Workforce Quality Insights
Use powerful analytics capabilities to generate end-to-end insights into how patient access activities are impacting the back-office outcomes.
Cost
Insights
Drill down into claims and encounter-level data to target and align controllable costs with outcomes and reimbursement.
Productivity
Analytics
Collect and deliver real-time insights on individual and collective registrar performance, and identify opportunities for training.








