
Compliance+
Amid a slew of compliance requirements, daily problems to solve, and overarching organizational goals, it can be difficult for provider organizations to organize improvement efforts and dedicate resources appropriately. Compliance+ is a complete workflow and analytics solution for compliance teams that need to proactively assess their at-risk claims, gain insights into ways to decrease mid-cycle denials, and show how their impact is affecting A/R trends.
Part of the Revenue Integrity Suite:
Connect compliance improvements to financial success and sustainability
Challenge
Solution
Basic reporting limits compliance team’s advancement
Challenge
Solution
Isolated data sets prevent benchmarking and comparisons
Analytics in action
Our intelligent platform and intuitive user interface make it easy to unlock the value of your data. In as little as three clicks, we bring meaningful insights, powerful visualization, and analytics innovation to help you make an even bigger impact at your organization.
Explore a few key features by hovering over the image.
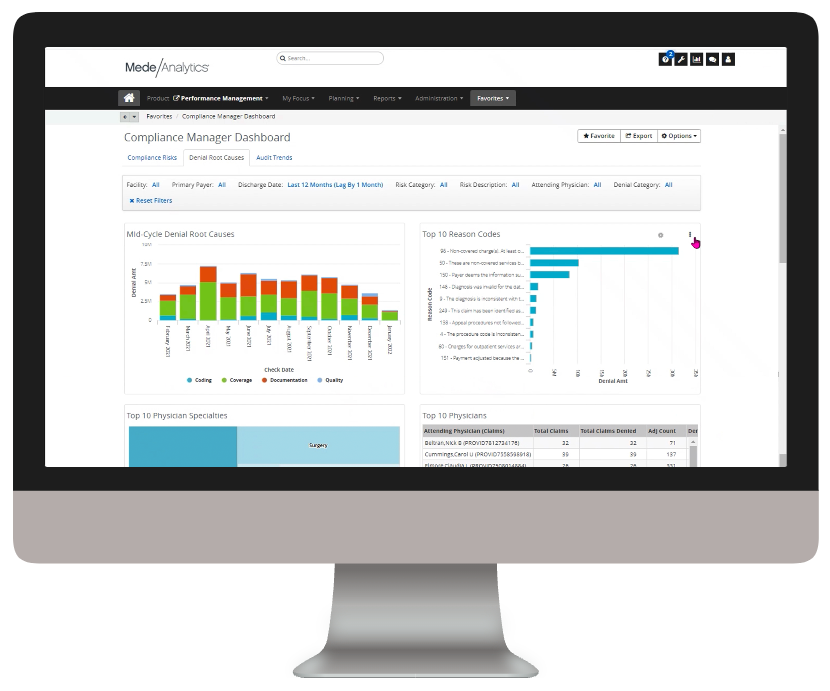
Gain insights into your at-risk claims, coding and documentation denials, and audit trends from a single dashboard
Quickly export reports and share insights on denial and audit trends
Filters allow for slicing and dicing without leaving your overview dashboard
Dive deeper into Compliance+
Download the data sheet to learn more about how Compliance+ saves hours in reporting.
Get our take on industry trends
Use SDOH + Analytics to power better outcomes for underserved population
Whether you’re a payer, provider or patient, on the front lines of care, sitting in front of a computer or receiving treatment, you’ve been affected by the pandemic. Of all the groups who participate in healthcare in one way or another, perhaps no single group has suffered more over the last year during the pandemic than the underserved— those people without ready access to needed healthcare services.
Read on...Go beyond recognition: Use data to take meaningful action this Nurses Week
Since 1994, America has observed National Nurses Week annually from May 6-12. This year more than ever before, it’s critical that healthcare organizations go beyond recognition and start taking action to more effectively support and serve nurses.
Read on...The future of digital health part 3: AI, machine learning and robotics
This post is part three of a new series featuring healthcare visionary and thought leader Andy Dé. In this series, Dé discusses how COVID-19 has triggered remarkable digital transformation and uncovers five, long-term innovation implications that providers, healthcare leaders, and payers need to consider.
Read on...The future of digital health part 2: Digital patient engagement and virtual healthcare delivery
Protecting the health, well-being and safety of healthcare practitioners and first responders is paramount — and will accelerate adoption of Digital Patient Engagement (DPE), enabled by Virtual Healthcare Delivery (VHD) solutions (also known as “Hospital at Home.)”
Read on...Want to talk with one of our experts?
Provider Value Analytics: Our full lineup of provider solutions
Everything you need to support your front office, mid-cycle and back office.
Patient
Access
Insights
Optimize patient satisfaction during the patient registration and payment clearance processes with critical, real-time analytics information.
Revenue Integrity
Suite
See how clinical operations affect your bottom line with complete visibility into compliance risk and clinical documentation performance.
Business Office
Suite
Achieve optimized cash flow and operational excellence with big-picture insight into opportunities for improving collection rate, denials, and staff productivity.

Workforce Quality Insights
Use powerful analytics capabilities to generate end-to-end insights into how patient access activities are impacting the back-office outcomes.
Cost
Insights
Drill down into claims and encounter-level data to target and align controllable costs with outcomes and reimbursement.
Productivity
Analytics
Collect and deliver real-time insights on individual and collective registrar performance, and identify opportunities for training.







