Network Insights
Monitor member coverage and provider outcomes to create high-performing provider networks
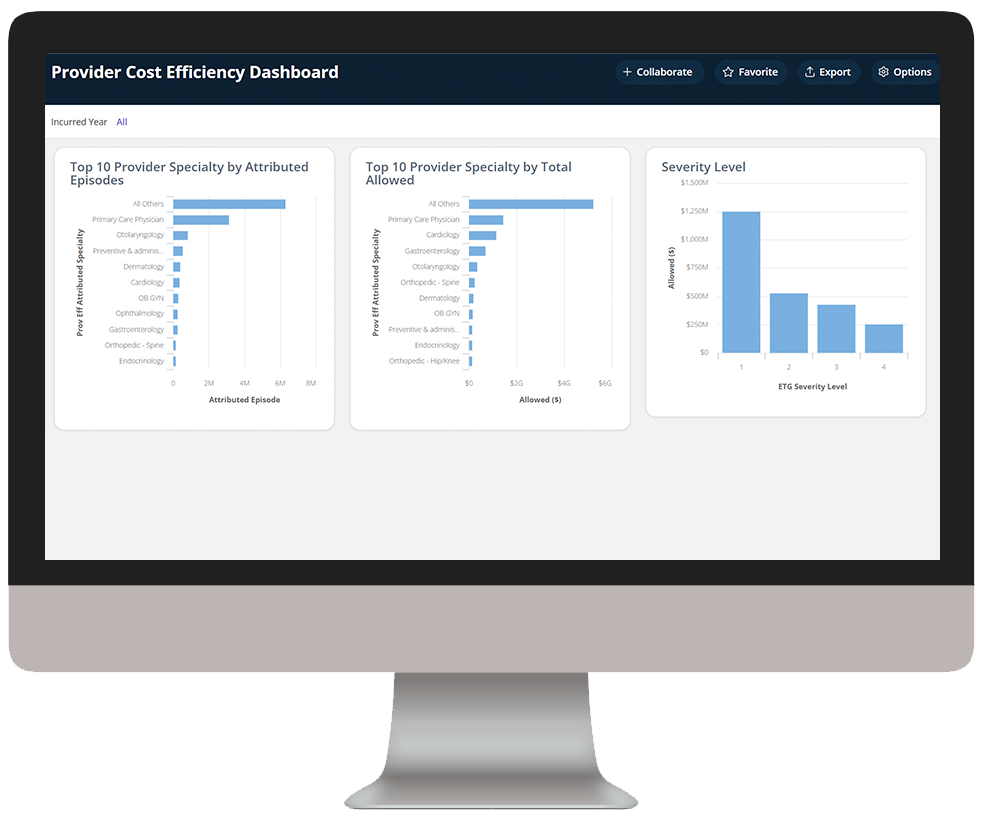
Executing network and provider performance analyses has historically been a very manual, time-consuming process with variable results. With value-based payment models expanding and focus on outcomes increasing, this method of monitoring is becoming obsolete. Smart health plans are replacing the manual work with automated, self-service analytics engines that offer an integrated view on network performance, provider patterns, cost of care and utilization trends.
Delivering comprehensive analytics solutions to strengthen your network
Challenge
Solution
Manual provider analysis processes consume significant time and resources unnecessarily
Challenge
Solution
Struggle to engage providers in performance improvement initiatives
Challenge
Solution
Difficulty adapting to value-based payment arrangements
Analytics in action
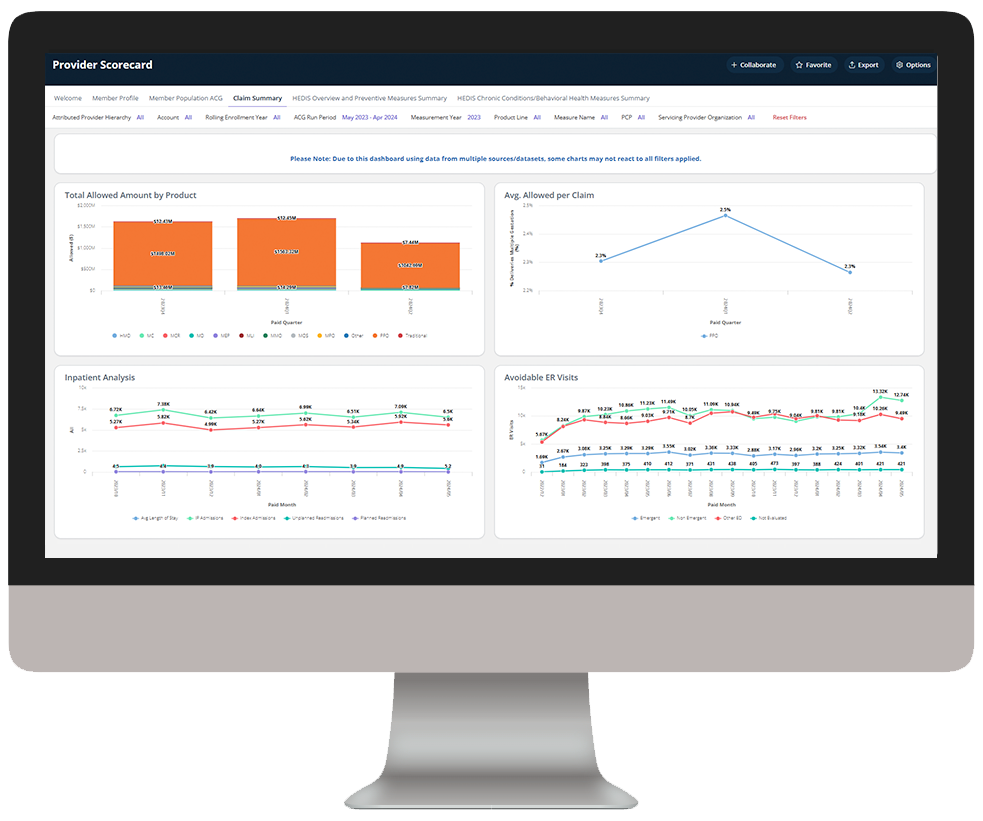
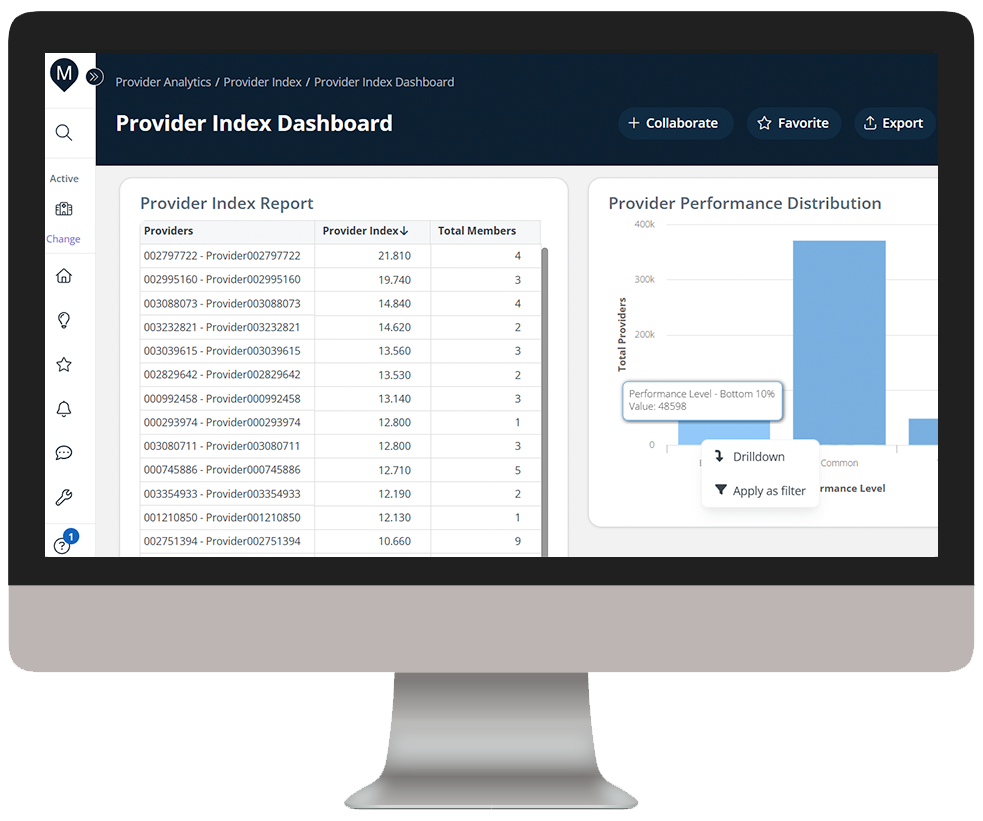
Our intelligent platform and intuitive user interface make it easy to unlock the value of your data. In as little as three clicks, we bring meaningful insights, powerful visualization, and analytics innovation to help you make an even bigger impact at your organization.
As you click through our example dashboards, hover over the image to explore a few key features.
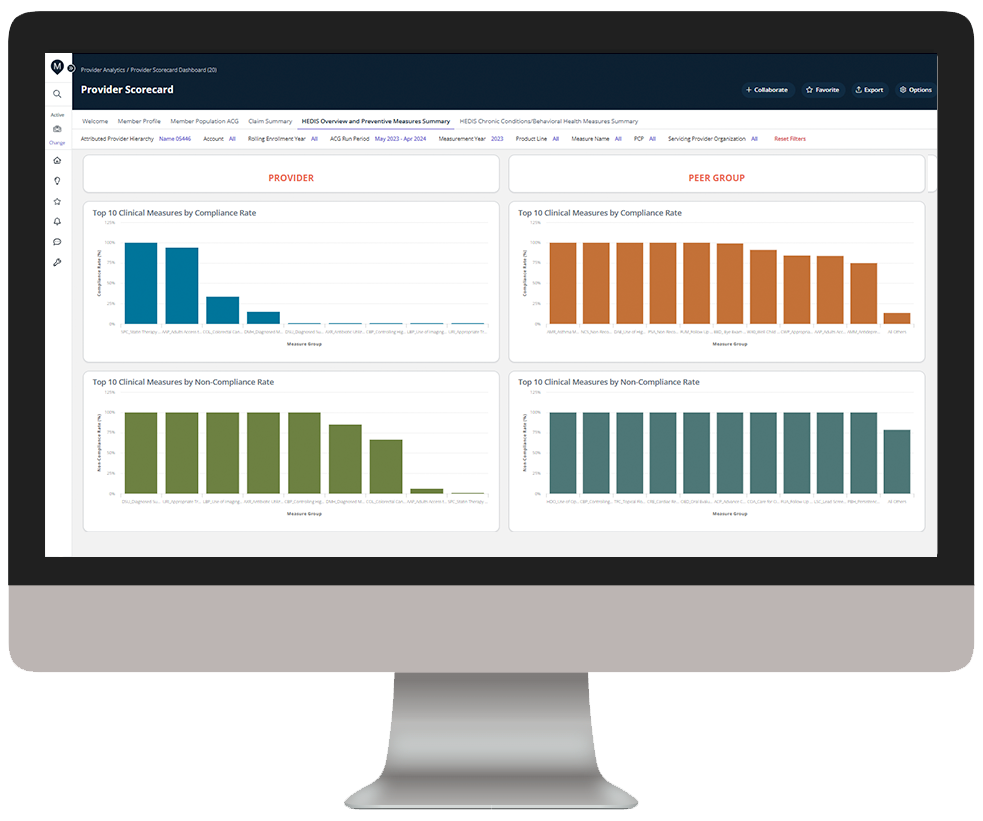
Compare provider performance against his/her peer group for the same measures
Drill down into provider details to identify performance improvement opportunities
Dive deeper into Network Insights
Download the data sheet to see how you can deploy Network Insights to build a strong network of the highest-performing providers.
Get our take on industry trends
2022 Rx: Your new, post-pandemic prescription for success
By Dave Schweppe, Chief Analytics Officer, MedeAnalytics Despite the common use of the term “post-COVID,” most leaders across the healthcare…
Read on...Combating the opioid epidemic in North America with Nobel Prize winning research
American Researchers Dr. David Julius and Dr. Ardem Patapoutian from California were awarded the Nobel Prize in medicine for their path breaking work on the development of non-opioid painkillers, showing immense promise for combating the epidemic.
Read on...Why managed Medicaid/Medicare health plans need analytics to improve outcomes
Managed care organizations that provide healthcare services to Medicare/Medicaid members are dedicated to improving the health and wellness of these underserved populations, especially those living in rural areas.
Read on...Using consumer analytics to steer health-related decisions
Companies tap into what people like to eat and drink, how we purchase consumables, where we like to shop, what shows we might like to stream, whether we vote, and so on. If you have ever created a profile on a streaming application (think Netflix or Amazon), you will receive recommended books, movies and other items just as soon as you start surfing.
Read on...Want to talk with one of our experts?
Payer Value Analytics: Our full lineup of payer solutions
Everything you need to step into the future of healthcare and drive real change across populations.
Quality Insights
Activate insights into population health and quality to improve satisfaction and outcomes for members and maintain a competitive position in the market.
Employer Insights
Elevate data sharing with employer groups to demonstrate plan value and increase efficacy of risk stratification and care management plans.
Network Insights
Accelerate provider performance with evidence-based outcomes comparisons, cost-effectiveness analyses, and extensive segmentation capabilities.