Medicaid Enterprise Analytics
Improving health management for your most at-risk members
With razor-thin margins on reimbursements and more value-based care at-risk contracts, health plans are clamoring for new and innovative ways to address the health of growing Medicaid populations. By mining insights from claim and clinical data, MedeAnalytics provides the foundation for managed care plans and agencies to collaborate and help deliver better outcomes to underserved populations.
Applying data to create person-centered care
Challenge
Solution
Lack of insight into actual impact of social determinants of health within membership limits efficacy of value-based care
Challenge
Solution
Disjointed data sources hinder understanding of member utilization trends and program outcomes
Challenge
Solution
Basic, low-detail view of member health statuses and population patterns stunts plan expansion
Analytics in action
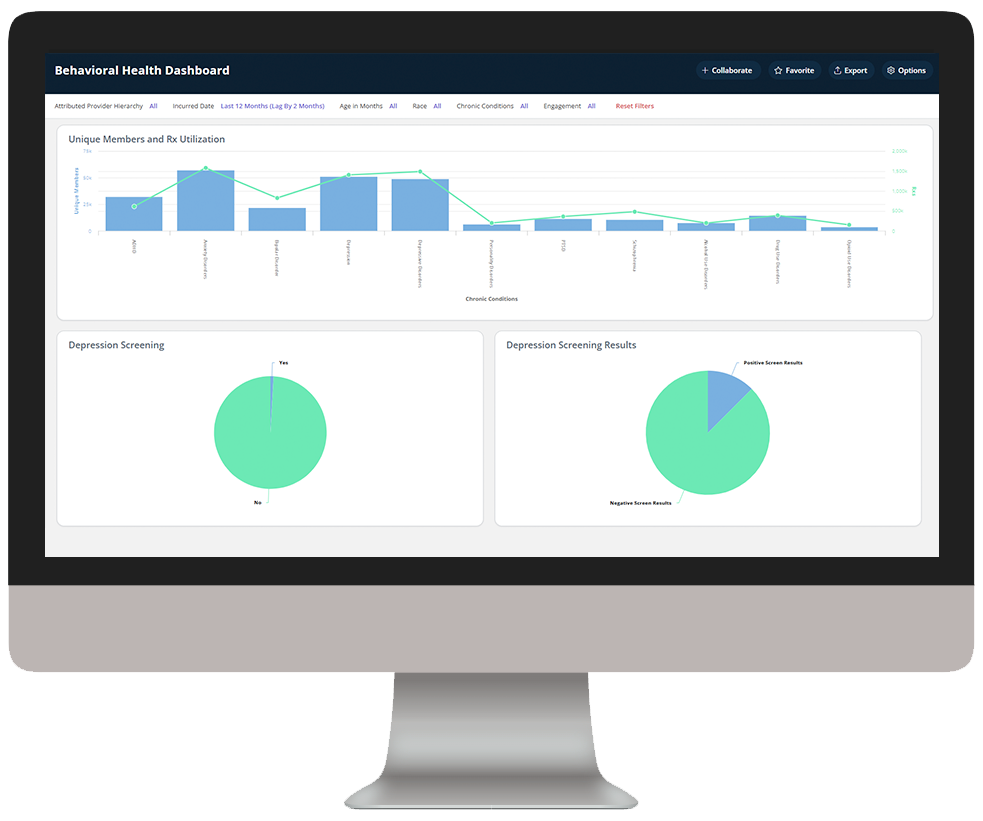
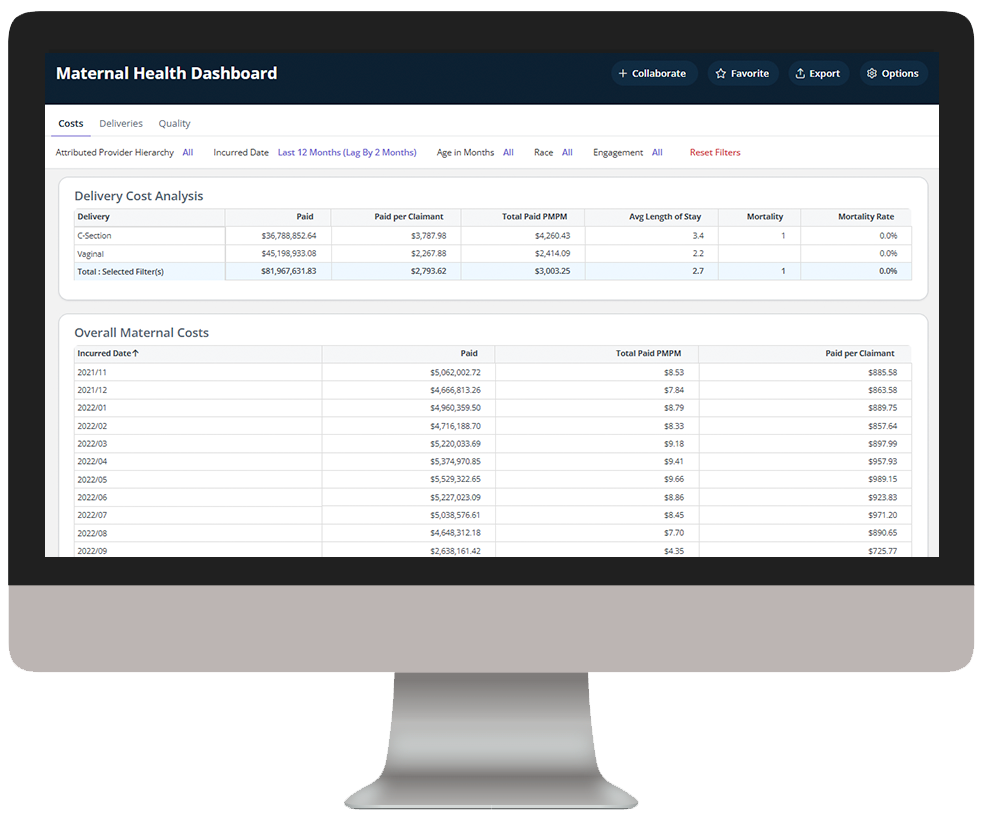
Medicaid Enterprise Analytics delivers key insights into Medicaid beneficiary data, enabling health plans to understand cost drivers, gaps in care, and demographic and SDOH impact to improve care outcomes.
Explore a few key features by hovering over the images below.
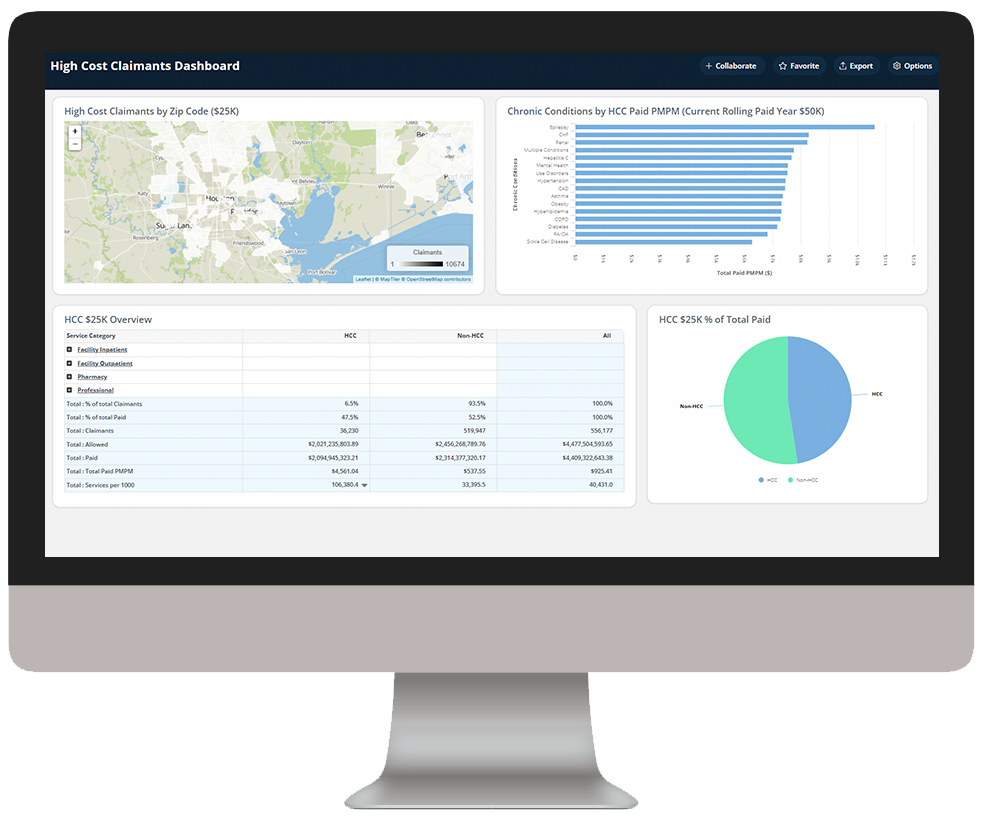
Identify high-cost claimants to prioritize for care management
Dive deeper into Medicaid Enterprise Analytics
Download the data sheet to see how Medicaid Enterprise Analytics integrates traditionally disparate data sources to provide the visibility and transparency health plans need to holistically manage member care.
Get our take on industry trends
3 ways to reduce friction in payer-provider relationships
The dynamic between healthcare providers and payers has historically been quite strained. Though both parties are interested in improving the…
Read on...Adapting nursing education and practice in a post-pandemic, technology-dependent world
Can AI help reduce nurse burnout? What role should nurses play in regulatory conversations? How do clinical training programs incorporate…
Read on...Championing transparent technology: Why we’ll always show you behind the scenes
Modern, tech-enabled innovations are demonstrating immense potential to transform the way healthcare is planned, delivered and paid for in the…
Read on...Optimize your revenue cycle for today’s challenges and tomorrow’s goals
In this dynamic LinkedIn Live discussion, Christine Stetler, BSN, RN and AVP of Solution Engineering at MedeAnalytics, unearthed strategies for…
Read on...Want to talk with one of our experts?
We're driving data-powered improvement across the industry

Healthcare providers and health systems
Healthcare Providers and Health Systems
use our end-to-end revenue cycle management analytics to lower denials, accelerate A/R, and improve staff productivity.

Healthcare payers and health plans
Healthcare Payers and health plans
deploy our value-based care and provider network analytics to enhance population health, quality and network management and empower their employers and brokers through self-service analytics.

Government Medicare and Medicaid programs
Government Medicare and Medicaid programs
Government Medicare and Medicaid programs rely on our comprehensive dashboards to understand cost drivers, gaps in care, and social determinants impacting beneficiary outcomes.