Medicaid Enterprise Analytics
Improving health management for your most at-risk members
With razor-thin margins on reimbursements and more value-based care at-risk contracts, health plans are clamoring for new and innovative ways to address the health of growing Medicaid populations. By mining insights from claim and clinical data, MedeAnalytics provides the foundation for managed care plans and agencies to collaborate and help deliver better outcomes to underserved populations.
Applying data to create person-centered care
Challenge
Solution
Lack of insight into actual impact of social determinants of health within membership limits efficacy of value-based care
Challenge
Solution
Disjointed data sources hinder understanding of member utilization trends and program outcomes
Challenge
Solution
Basic, low-detail view of member health statuses and population patterns stunts plan expansion
Analytics in action
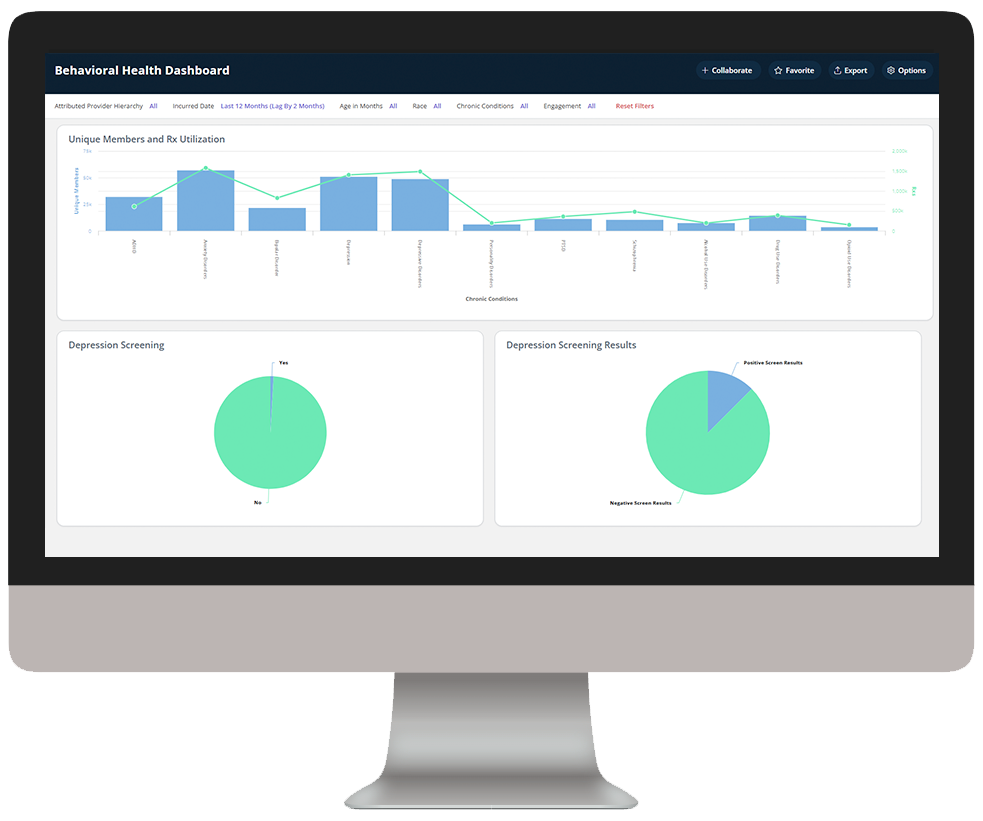
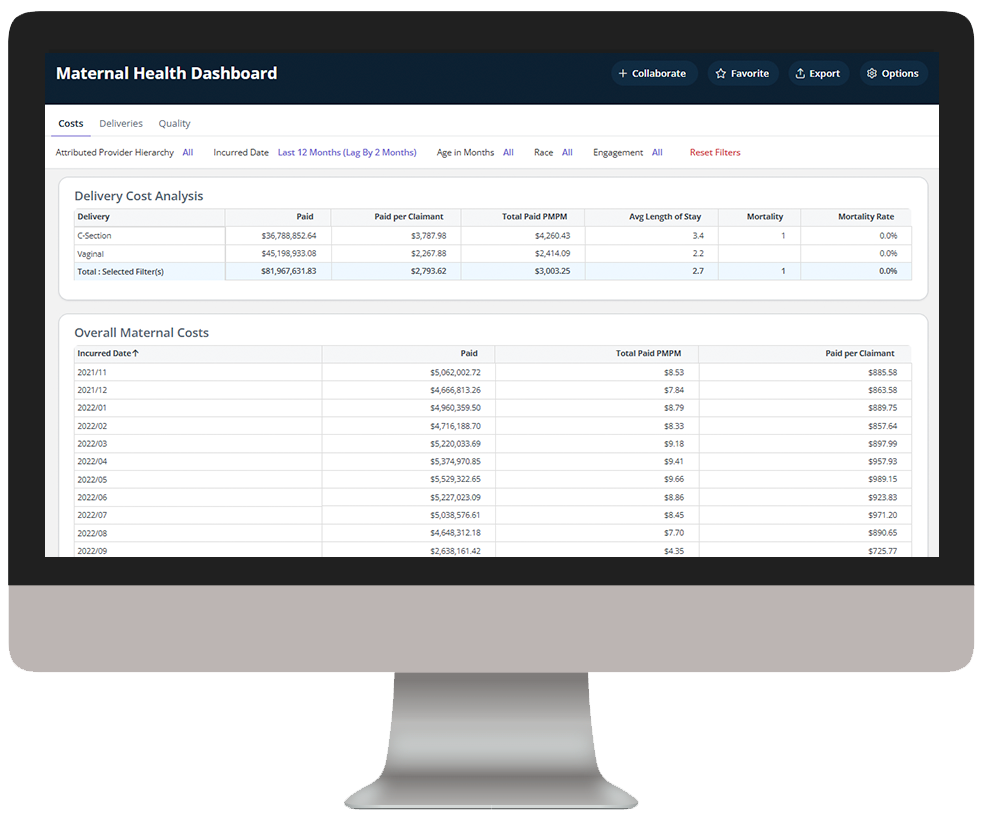
Medicaid Enterprise Analytics delivers key insights into Medicaid beneficiary data, enabling health plans to understand cost drivers, gaps in care, and demographic and SDOH impact to improve care outcomes.
Explore a few key features by hovering over the images below.
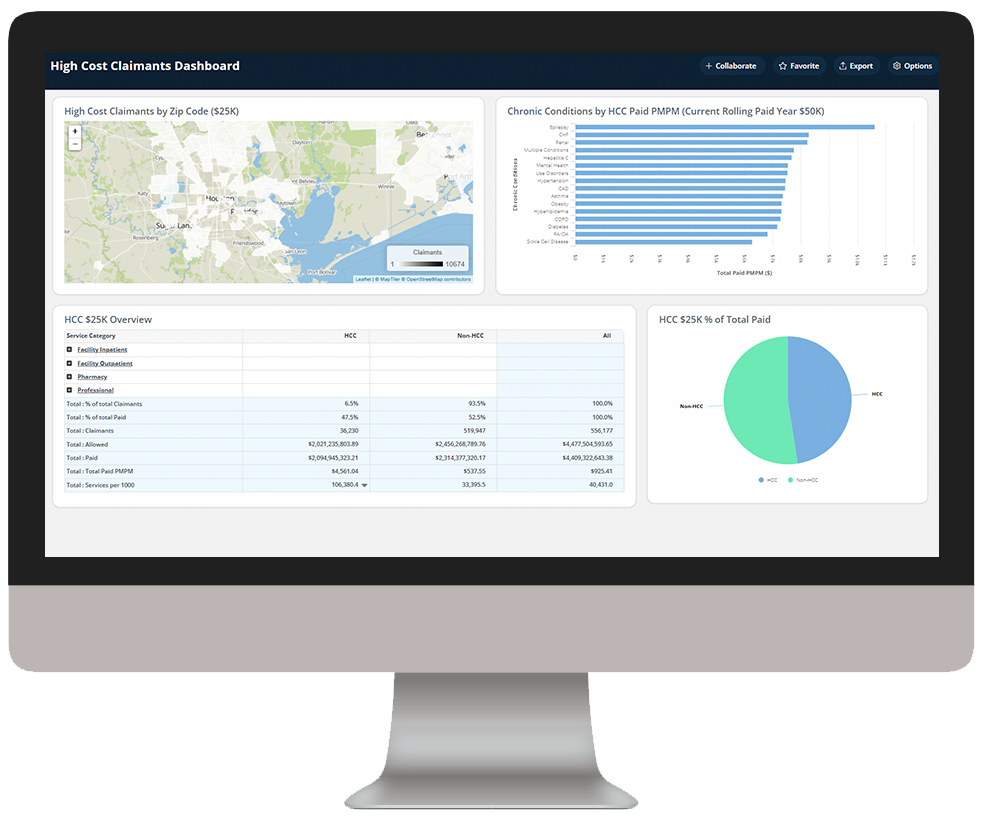
Identify high-cost claimants to prioritize for care management
Dive deeper into Medicaid Enterprise Analytics
Download the data sheet to see how Medicaid Enterprise Analytics integrates traditionally disparate data sources to provide the visibility and transparency health plans need to holistically manage member care.
Get our take on industry trends
Measuring provider cost and utilization
No matter the time of year, payers and providers should work to agree on a shared source of truth when it comes to data. With the recent end of the year, it’s time to celebrate the new year (who isn’t ready to say goodbye to 2020?) and close the books, which includes the reconciliation of any shared savings or losses.
Read on...Data visualization: A picture is worth a thousand…healthcare data points?
The amount of data produced daily has grown exponentially with nearly 90% of the world’s data generated in the last two years alone. To ensure we can make sense of this data, analysts must find meaningful ways to present the information to their audiences.
Read on...How to help employer groups plan in a time of uncertainty
Employers and their sponsored health plans are thinking about next year’s benefit designs with a significant challenge not seen before: the effect of the coronavirus pandemic. There are important considerations to take into account before making any decisions about new or existing coverage. Becky Niehus, a director of Product Consulting at MedeAnalytics, explores these new issues and what employers can do to ensure employees are “covered.”
Read on...Healthcare’s return to “normal” after COVID-19: Is it possible?
As providers determine how to get patients to return to facilities for routine disease management and preventive screenings, opportunities are ripe for the application of analytics to triage at the right time to the right setting. Data related to COVID-19 will continue to flow rapidly, but there are possibly more questions than answers now about a return to “normal.”
Read on...Want to talk with one of our experts?
We're driving data-powered improvement across the industry

Healthcare providers and health systems
Healthcare Providers and Health Systems
use our end-to-end revenue cycle management analytics to lower denials, accelerate A/R, and improve staff productivity.

Healthcare payers and health plans
Healthcare Payers and health plans
deploy our value-based care and provider network analytics to enhance population health, quality and network management and empower their employers and brokers through self-service analytics.

Government Medicare and Medicaid programs
Government Medicare and Medicaid programs
Government Medicare and Medicaid programs rely on our comprehensive dashboards to understand cost drivers, gaps in care, and social determinants impacting beneficiary outcomes.