Part 4
This post is the fourth and final of our Digital Health series, featuring healthcare visionary and thought leader Andy Dé. In this series, Dé has been discussing how COVID-19 has triggered remarkable digital transformation and uncovers five long-term innovation implications that providers, healthcare leaders, and payers need to consider.
To catch up on the previous three posts, navigate to the following links:
– Innovation implication #1: Advanced analytics for vaccine administration
– Innovation implication #2: Digital patient engagement and virtual healthcare delivery
Then, read on to explore today’s topic: Artificial Intelligence and analytics.
Innovation implication #5: Convergence of AI and analytics for healthcare payers
Healthcare payers are experiencing tremendous, pandemic-driven cost pressures as well as unprecedented changes to their reimbursement mixes (thanks to the explosive growth of telehealth and similar services). To stay successful, I predict payers will extensively leverage advanced descriptive, spatial, predictive and prescriptive analytics driven by a convergence of analytics and artificial intelligence comprising machine learning, natural language processing, and deep learning.
In this post, I’ll follow the strategy framework laid out in the below graphic and detail each high value area of potential investment in advanced analytics.
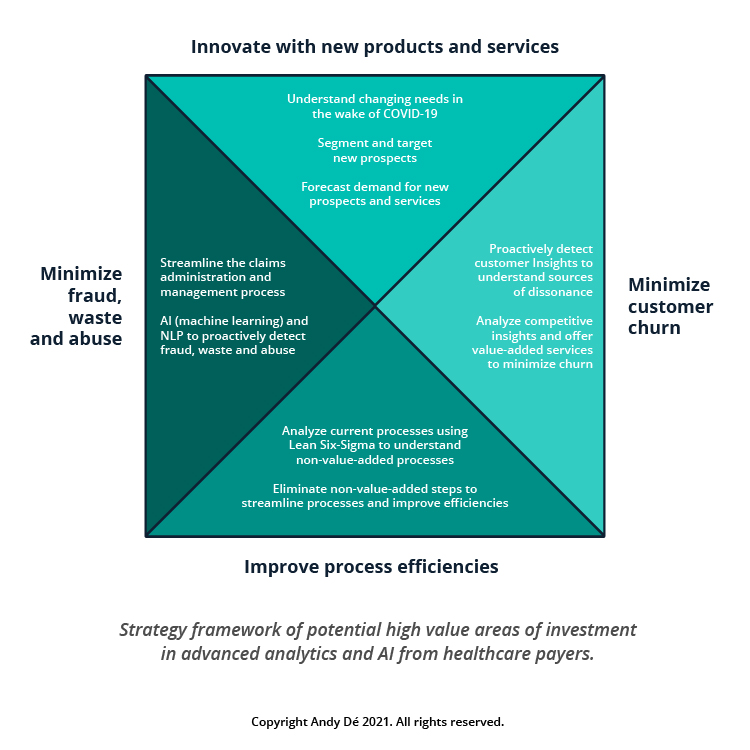
1. Innovate with new products and services for new segments of customers
The COVID-19 pandemic and the resulting economic catastrophe has caused millions of Americans to be laid off or furloughed – usually losing employer provided health coverage as a result.
Simultaneously, 32.8 million Americans have been infected by COVID-19 as of today and many will suffer long-term physical effects of the virus. COVID-19 has become a “pre-existing condition” for these afflicted patients.
Deploying advanced analytics and AI will help payers identify the changing needs of their customers and respond to their evolving needs with newer products and services that will enable new revenue streams to compensate for lost revenue.
2. Minimize customer churn through value-added programs
Advanced predictive and prescriptive analytics have helped large healthcare payers to better understand their customer behavior, address dissonance with their products and services and deploy value-added programs to minimize customer churn. These steps have helped protect millions in revenue, which would otherwise have been lost.
3. Improve process efficiencies
Healthcare payers are also challenged with several administrative processes which are manual, inefficient, onerous and can negatively impact employee morale (e.g., claims administration and management).
I foresee industry leaders deploying best practices like analytics- and AI-enabled Lean Six-Sigma for value stream mapping to stratify current processes in terms of value-add vs. non-value-add process steps from the customer’s perspective. This will enable them to eliminate non-value-add processes or steps, enhancing process efficiency, customer satisfaction and employee productivity – and saving millions in costs.
4. Minimize fraud, waste and abuse for millions in cost savings
Fraudulent claims filed on behalf of patients by unscrupulous physicians, providers and predatory pharmacies is a significant challenge, which costs healthcare payers billions in leakage every year.
Deploying advanced machine learning and natural language processing algorithms with analytic automation will help payers to proactively flag and detect fraud, identify waste and abuse pertaining to claims administration, management and reimbursement – and save them millions in leakage and cost savings each year.
This concludes our series on the future of digital health. Thank you for following along!
I hope you’ve learned key insights and gained actionable takeaways that can be incorporated into your strategic plans and preparation pathways. To discuss any of these implications further, reach out to start the conversation. Let’s innovate together!
Get our take on industry trends
Why Unconventional Businesses Will Find Success in Healthcare: It’s the Data
It seems everyone is moving into healthcare. It’s a rapidly growing industry, historically dominated by large, well-embedded companies and organizations, and “pure tech” companies have had difficulty breaking in. That, however, is changing.
Read on...Data and Social Determinants of Health
By Scott Hampel – I think a lot–and I’m not the only one–about how we can improve the ways we pull information from data. Data on its own is inert: just waiting to be understood and then used. And that’s a major challenge for many organizations. Data is often trapped in different applications with no easy or convenient way to extract it.
Read on...Why Social Determinants Need Analytics for Success
Many challenges face healthcare’s underserved. There are issues with food, housing, reliable transportation, steady employment and more. Each contributes to and is one element of social determinants of health (SDH). In communities around the world, public and private organizations are taking steps to address SDH-related issues and challenges that negatively impact healthcare.
Read on...Healthcare Organizations Recognize Importance of AI for Reporting
Healthcare providers continue to recognize the value of using AI in reporting operations throughout the organization. AI has many strengths when applied to the healthcare industry:
Read on...


