Part 4
This post is the fourth and final of our Digital Health series, featuring healthcare visionary and thought leader Andy Dé. In this series, Dé has been discussing how COVID-19 has triggered remarkable digital transformation and uncovers five long-term innovation implications that providers, healthcare leaders, and payers need to consider.
To catch up on the previous three posts, navigate to the following links:
– Innovation implication #1: Advanced analytics for vaccine administration
– Innovation implication #2: Digital patient engagement and virtual healthcare delivery
Then, read on to explore today’s topic: Artificial Intelligence and analytics.
Innovation implication #5: Convergence of AI and analytics for healthcare payers
Healthcare payers are experiencing tremendous, pandemic-driven cost pressures as well as unprecedented changes to their reimbursement mixes (thanks to the explosive growth of telehealth and similar services). To stay successful, I predict payers will extensively leverage advanced descriptive, spatial, predictive and prescriptive analytics driven by a convergence of analytics and artificial intelligence comprising machine learning, natural language processing, and deep learning.
In this post, I’ll follow the strategy framework laid out in the below graphic and detail each high value area of potential investment in advanced analytics.
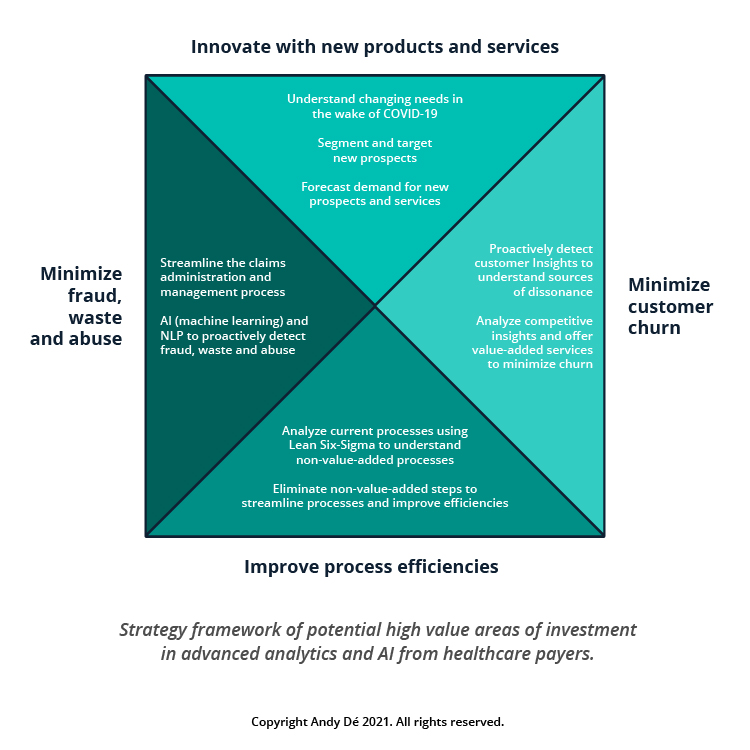
1. Innovate with new products and services for new segments of customers
The COVID-19 pandemic and the resulting economic catastrophe has caused millions of Americans to be laid off or furloughed – usually losing employer provided health coverage as a result.
Simultaneously, 32.8 million Americans have been infected by COVID-19 as of today and many will suffer long-term physical effects of the virus. COVID-19 has become a “pre-existing condition” for these afflicted patients.
Deploying advanced analytics and AI will help payers identify the changing needs of their customers and respond to their evolving needs with newer products and services that will enable new revenue streams to compensate for lost revenue.
2. Minimize customer churn through value-added programs
Advanced predictive and prescriptive analytics have helped large healthcare payers to better understand their customer behavior, address dissonance with their products and services and deploy value-added programs to minimize customer churn. These steps have helped protect millions in revenue, which would otherwise have been lost.
3. Improve process efficiencies
Healthcare payers are also challenged with several administrative processes which are manual, inefficient, onerous and can negatively impact employee morale (e.g., claims administration and management).
I foresee industry leaders deploying best practices like analytics- and AI-enabled Lean Six-Sigma for value stream mapping to stratify current processes in terms of value-add vs. non-value-add process steps from the customer’s perspective. This will enable them to eliminate non-value-add processes or steps, enhancing process efficiency, customer satisfaction and employee productivity – and saving millions in costs.
4. Minimize fraud, waste and abuse for millions in cost savings
Fraudulent claims filed on behalf of patients by unscrupulous physicians, providers and predatory pharmacies is a significant challenge, which costs healthcare payers billions in leakage every year.
Deploying advanced machine learning and natural language processing algorithms with analytic automation will help payers to proactively flag and detect fraud, identify waste and abuse pertaining to claims administration, management and reimbursement – and save them millions in leakage and cost savings each year.
This concludes our series on the future of digital health. Thank you for following along!
I hope you’ve learned key insights and gained actionable takeaways that can be incorporated into your strategic plans and preparation pathways. To discuss any of these implications further, reach out to start the conversation. Let’s innovate together!
Get our take on industry trends
Helping Accountable Care Organizations Navigate the Perfect Storm
In the ever-evolving landscape of healthcare, Accountable Care Organizations (ACOs) find themselves at the epicenter of a transformative era. Recently,…
Read on...Navigating the Medicare Landscape: Implications of the Latest Rule Changes for Healthcare Organizations
The Centers for Medicare & Medicaid Services (CMS) has recently unveiled significant proposed changes to Medicare Advantage (MA), Medicare Prescription…
Read on...Introduction to social risk: What healthcare leaders need to understand
‘Social determinants of health’ has been a common phrase for decades now, but the term social risk is much less…
Read on...AI is your new crystal ball: How predictive analytics can reduce denials
The idea of having a crystal ball to better understand what claims will be denied is an awesome concept. But one we can’t rely on. Thankfully, we have predictive analytics to take the place of a crystal ball.
Read on...


