As much as the past 18 months of pandemic disruption have compromised staffing operations, financial stability, patient care, customer service, and many other facets of healthcare, we are also witnessing unique opportunities for transformation emerging in these spaces.
Let’s take a look at a few of the top challenges for healthcare payers, as well as the unique opportunities they bring.
- Rising healthcare costs: Payers need self-service analytics to empower their employer clientele and their brokers to understand, mitigate and explain costs at the executive and user levels, without constant support from their IT organizations. Analytics need to enable health plans to identify underlying root causes and take action to improve performance.
- Declining commercial membership: Health plans need to demonstrate the value of their plans to their employer clientele and brokers to be perceived as ”trusted advisors.” Only when value is recognized and capitalized on can they improve loyalty, retention and revenue uplift.
- Increasing provider consolidation: Health plans are no longer able to dictate terms of provider payment arrangements. But they still have an imperative to reduce the total cost of care through provider network management and increased provider participation in value-based care programs. To accomplish this, they need comparative data to effectively structure contracts and negotiate with providers.
To help payers take advantage of the opportunity to address these challenges, they need to:
- Provide employers with an integrated view of plan performance
- Get actionable insights into drivers of care cost and quality
- Deploy customized self-service reports and presentations with KPIs and metrics
That’s where MedeAnalytics Employer Reporting plugs in.
One excellent illustration I wanted to share with you is the compelling story of Blue Cross & Blue Shield of Rhode Island (BCBSRI). This organization was challenged with a lack of actionable employer insights and reporting, which negatively impacted customer retention and acquisition. Report turnaround times (TAT) were in excess of 2-3 weeks, which was not sustainable or acceptable for customers.
In a recent webinar, Angelo Pirri, manager of Employer Analytics at BCBSRI articulated how the health plan deployed MedeAnalytics Employer Reporting to empower their consultants to collaborate directly with brokers as "trusted advisors” using the following capabilities:
- 360-degree view that provides a “single version of the truth” for the customers
- Easily identified opportunities for standardization, cost savings and performance improvement
- Quick report turnaround time (hours vs. weeks)
This value-added self-service analytics solution also helped BCBSRI craft multi-year strategies based on fact-based data and insights for their strategic clientele, driving up employer efficiencies while significantly augmenting new client acquisition and satisfaction.
Some of the key lessons learned from the analytics deployment were:
- Having a clear strategy and ambitious yet manageable goals for outcomes
- Focus on value to customers, executives and internal stakeholders that will pay back on the investments
- Deployment takes time; have realistic expectations
- Given the efficiency and productivity enhancements from the Mede solutions, think through how the role of the analyst will evolve to support value-added services
These transformative changes and lessons learned helped BCBSRI improve customer satisfaction and halt the loss of strategic clients to the competition—as well as gain back many major clients that had left in prior years. The Employer Reporting solution also led to a dramatic improvement in information consultants’ productivity and morale, given their perception as “trusted advisors” by brokers and their employers.
As always, numbers help paint the picture in full, vibrant color. BCBSRI’s work with MedeAnalytics resulted in measurable value and outcomes, including:
- 50% reduction in Standard Reports Turn-Around-Times (TAT)
- 75% reduction in Ad-Hoc Reports Turn-Around-Times (TAT)
- 11.6 months payback on the investment in the employer reporting solution
- $2.9 million in increased efficiencies and revenue uplift culminating from the solution
To learn more about this story and solution, I encourage you to watch the webinar playback.
Get our take on industry trends
Best practice tools to build an integrated approach to multimorbidity
The traditional model of treating single diseases no longer works. Data collected from 2016 to 2019 indicated that 32.9% of…
Read on...Will adopting a risk-based approach with augmented analytics support care gap closure?
A common challenge for healthcare systems is how to properly segment its patient populations based on risk profiles and co-morbidities. Doing this well ensures a high quality of care delivery and superior patient outcomes.
Read on...4 questions healthcare executives are asking about augmented analytics
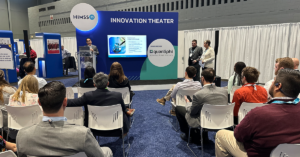
At our annual Impact Summit, I had the privilege to talk about augmented analytics and address questions from healthcare executives—many…
Read on...