Pioneering payers know that building a strong foundation is the key to enacting sustainable innovation. This foundation typically includes the following handful of elements:
- Depth and breadth of expertise
- Persistent feedback loop
- Close customer relationships
- Leaders invested in growth and vision
- Dedicated innovation team
This solid base is critical to surviving the constant intensity and pressure of the healthcare industry. We’ve seen this play out on a global stage over the past two years of living in COVID-19 times.
In this blog post, I’ll explore pandemic-driven trends affecting health plans’ foundations, analytics-driven answers to their challenges, and experience-driven predictions for what’s on the innovation horizon.
Pandemic-driven trends
For health plans specifically, new or augmented trends from the pandemic include:
- Consumers deferring care and preventative screenings
- Patients choosing virtual care settings over in-person sites
- Pandemic trackers highlighting inequities and disparities across the industry
- Data transparency taking priority in many healthcare organizations
- Financial pressure looming for providers, payers, businesses and consumers
- Vaccination status determining availability of certain services and rates
To capitalize on the opportunities and tackle the challenges presented by such trends, health plans need to take a strategic, data-based approach. Take a look at a few examples of payers that partnered with MedeAnalytics to develop and execute this approach.
Analytics-driven answers
ConcertoCare
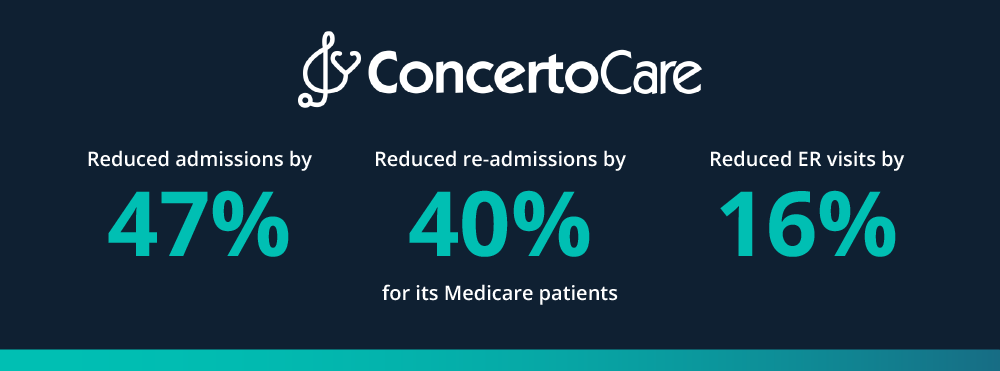
ConcertoCare came to MedeAnalytics looking to address vulnerable populations more effectively. They wanted to reduce their hospital admissions for specific targeted groups and segment their population for more effective care management. Utilizing our Population Health solution, ConcertoCare was able to stratify risk and assess the cost and utilization patterns across their entire population. Get the full story
BlueCross & BlueShield of Rhode Island (BCBSRI)

BCBSRI was experiencing challenges with their employer reporting. Though they were information-rich, their information was siloed and difficult to manage. Customer attrition was rising quickly, mainly due to lack of insights and quality reporting. With MedeAnalytics’ Employer Reporting solution, BCBSRI began providing real-time, actionable data to brokers and employers, and evolving their analysts into trusted advisors. Get the full story
Experience-driven predictions
I have spent over 25 years—nearly my entire career—dedicated to understanding and improving the healthcare ecosystem in America. In that time, I’ve had the pleasure of working alongside and partnering with many incredible minds that have shaped my outlook on where healthcare is headed. Now with MedeAnalytics, I am excited for the opportunity to be on the frontlines of the industry’s digital transformation.
Here’s what I see on the horizon for innovation in payer analytics:
- Increase in usability of data: New cohorting and benchmarking advancements will provide the actionable insights payers need into social determinants of health, consumer behavior, and other specific metrics.
- More self-service capabilities: Simple—yet powerful—configuration options within analytics solutions will enable health plans to achieve greater scalability, faster time to value, and higher degree of satisfaction.
- Expansion beyond software: Robust consulting and support services will allow health plans to make the most out of their analytics investments and improve overall performance.
- Exchange of insights, inspiration: Payers will begin engaging with each other more to improve the health and wellbeing of people across the nation. The pandemic forced many unlikely partnerships, which ultimately yielded meaningful outcomes, and there is vast opportunity to continue that type of collaboration.
As every year does, I am sure 2022 will bring its own unexpected twists and turns, and payers will be required to adapt in order to survive and thrive. One thing will stay the same, however. MedeAnalytics will continue dedicating all our time and effort to developing analytics solutions and services that empower you to continue innovating, perform at your best, and create measurable impact across the industry.
Get our take on industry trends
Five predictions for healthcare analytics and AI
Healthcare leaders increasingly realize the tremendous potential in artificial intelligence (AI) and analytics to deliver on the promise of high-quality…
Read on...


