Value-Based Care Administration
Implement purpose-built infrastructure for
value-based care networks
Value-based care networks are composed of many multifaceted and interdependent entities that must work collaboratively to be successful. This many-to-many system of relationships is complex to navigate. Healthcare organizations need an integrated, configurable data platform with end-to-end management to simplify and streamline efforts.
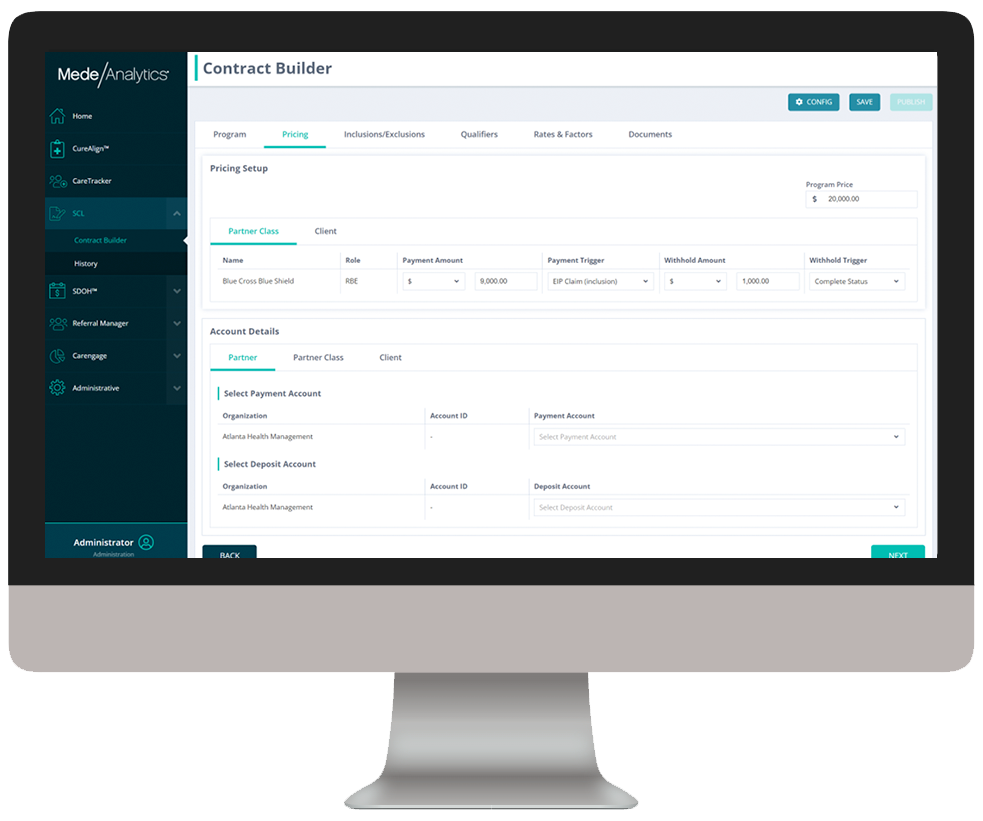
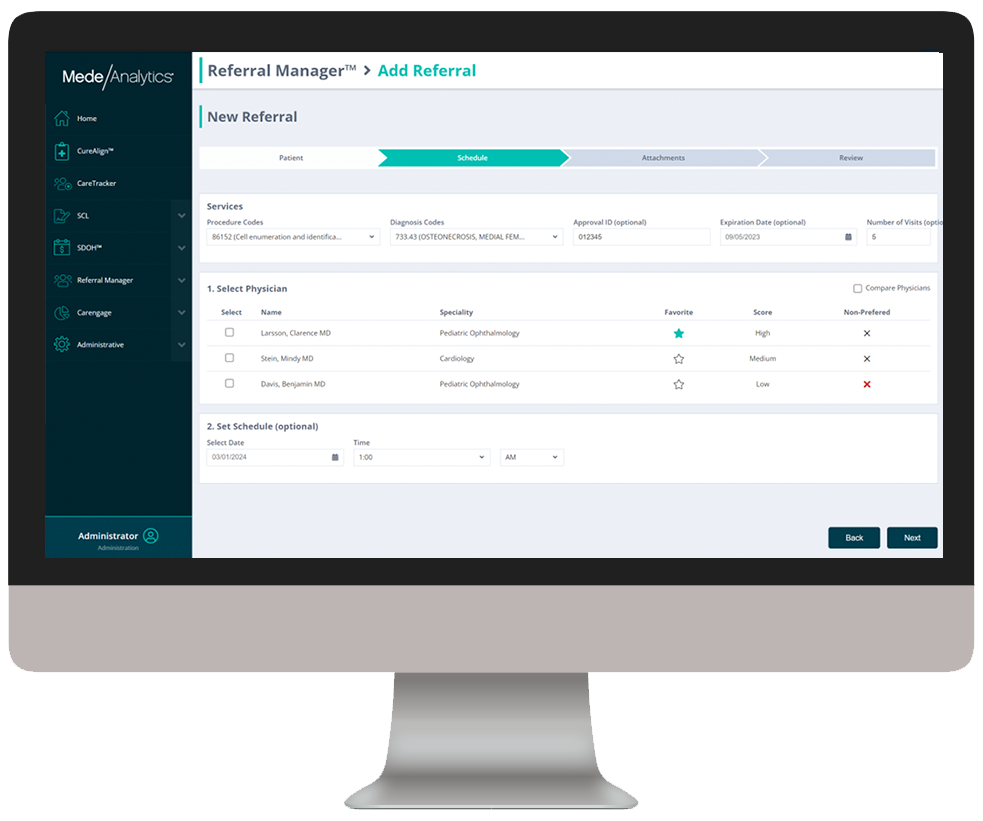
Using robust contract management and financial payment capabilities, payers and providers can realign downstream reimbursement, incorporate SDOH resources, and demonstrate real-time performance impact with robust dashboards. By melding value-based reimbursement programs with whole-person health models, you can deliver higher quality care, significantly reduce costs, and streamline fund transfers.
Build a patient-centric, service-focused approach to precision health challenge
Challenge
Solution
Legacy data systems are not able to utilize the unstructured data (charts, notes, images, etc.) that produces and informs actionable insights
Challenge
Solution
Traditional approaches do not support the "network of networks" infrastructure that allows scaling of value-based contracts and/or payment model adoption
Challenge
Solution
Lack of timeliness, transparency and advanced analytics in legacy systems hinders productivity, accountability and decision-making
Behind the scenes
We’ve partnered with HSBlox, an industry-leading contract and payment management organization, to empower you with the tools and support necessary to deliver value-based care successfully and sustainably in a single solution.
Read the press release to see how we are working together to enhance value-based care outcomes with data-driven insights, performance optimization, and seamless fund transfers as part of the industry’s most complete value-based care management solution.
Analytics in action
Value-Based Care Administration combines powerful analytics with contract and payment management capabilities to enhance VBC outcomes through data-driven insights, performance optimization, and seamless funds transfers.
As you click through our example dashboards, hover over the image to explore a few key features.
Visualize patient-level program tracking from start to finish
Dive deeper into Value-Based Care Administration
Download the data sheet to see how Value-Based Care Administration helps:
- Payers optimize networks, track performance, and manage contracts
- Providers evaluate quality, improve payer relationships, and streamline payments
Get our take on industry trends
Helping Accountable Care Organizations Navigate the Perfect Storm
In the ever-evolving landscape of healthcare, Accountable Care Organizations (ACOs) find themselves at the epicenter of a transformative era. Recently,…
Read on...Navigating the Medicare Landscape: Implications of the Latest Rule Changes for Healthcare Organizations
The Centers for Medicare & Medicaid Services (CMS) has recently unveiled significant proposed changes to Medicare Advantage (MA), Medicare Prescription…
Read on...Introduction to social risk: What healthcare leaders need to understand
‘Social determinants of health’ has been a common phrase for decades now, but the term social risk is much less…
Read on...AI is your new crystal ball: How predictive analytics can reduce denials
The idea of having a crystal ball to better understand what claims will be denied is an awesome concept. But one we can’t rely on. Thankfully, we have predictive analytics to take the place of a crystal ball.
Read on...Want to talk with one of our experts?
We're driving data-powered improvement across the industry

Healthcare payers and health plans
Healthcare Payers and health plans
deploy our value-based care and provider network analytics to enhance population health, quality and network management and empower their employers and brokers through self-service analytics.

Healthcare providers and health systems
Healthcare Providers and Health Systems
use our end-to-end revenue cycle management analytics to lower denials, accelerate A/R, and improve staff productivity.

Government Medicare and Medicaid programs
Government Medicare and Medicaid programs rely on our comprehensive dashboards to understand cost drivers, gaps in care, and social determinants impacting beneficiary outcomes.