Quality Insights
Improve value-based care quality and population health outcomes
The rise of value-based care has inevitably spurred heightened focus on quality improvement across the healthcare ecosystem. There are two sides to this coin: measures and members. On the measures side, health plans are working to align with strict national standards and state-specific requirements (think: HEDIS, Star ratings). On the members side, payers are striving to understand their patient populations more fully and provide more timely, appropriate interventions.
Delivering comprehensive solutions to enhance performance and outcomes
Challenge
Solution
Siloed, incompatible information from EMRs, claims and other sources hinder efficient quality calculations and data submission
Challenge
Solution
Unnecessary ED visits and readmissions drive up costs and decrease member satisfaction
Challenge
Solution
Insufficient, unreliable data on clinical performance deters provider engagement
Celebrating big wins with Quality Insights
Analytics in action
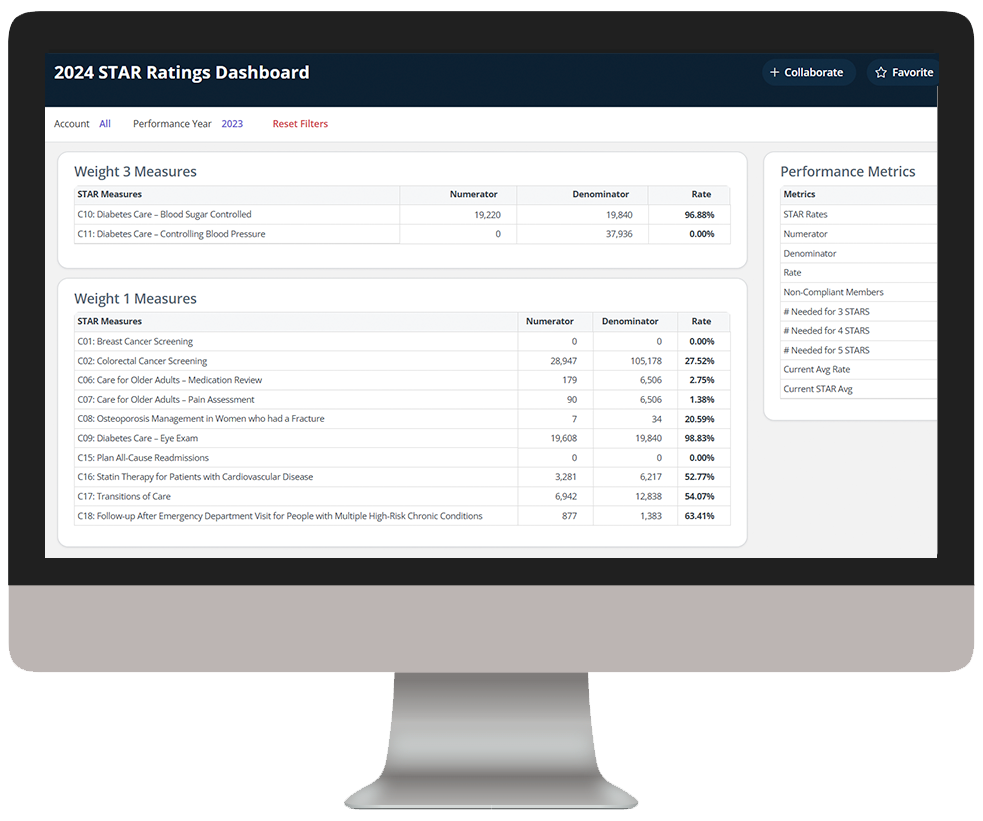
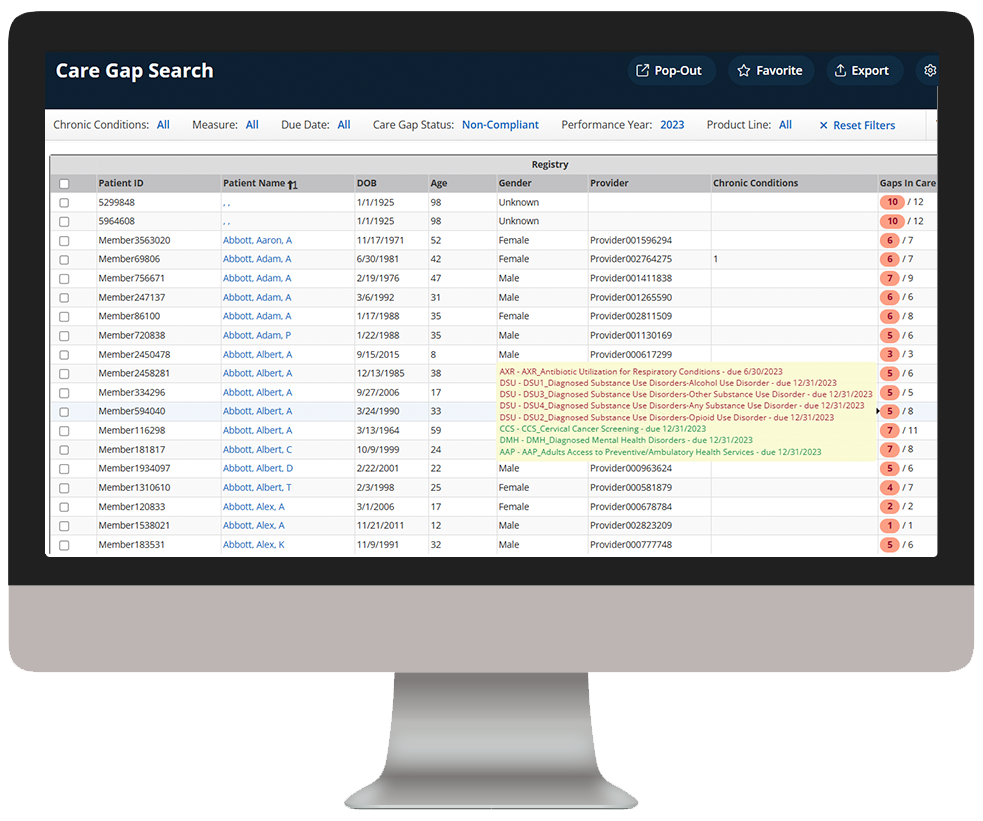
Our intelligent platform and intuitive user interface make it easy to unlock the value of your data. In as little as three clicks, we bring meaningful insights, powerful visualization, and analytics innovation to help you make an even bigger impact at your organization.
As you click through our example dashboards, hover over the image to explore a few key features.
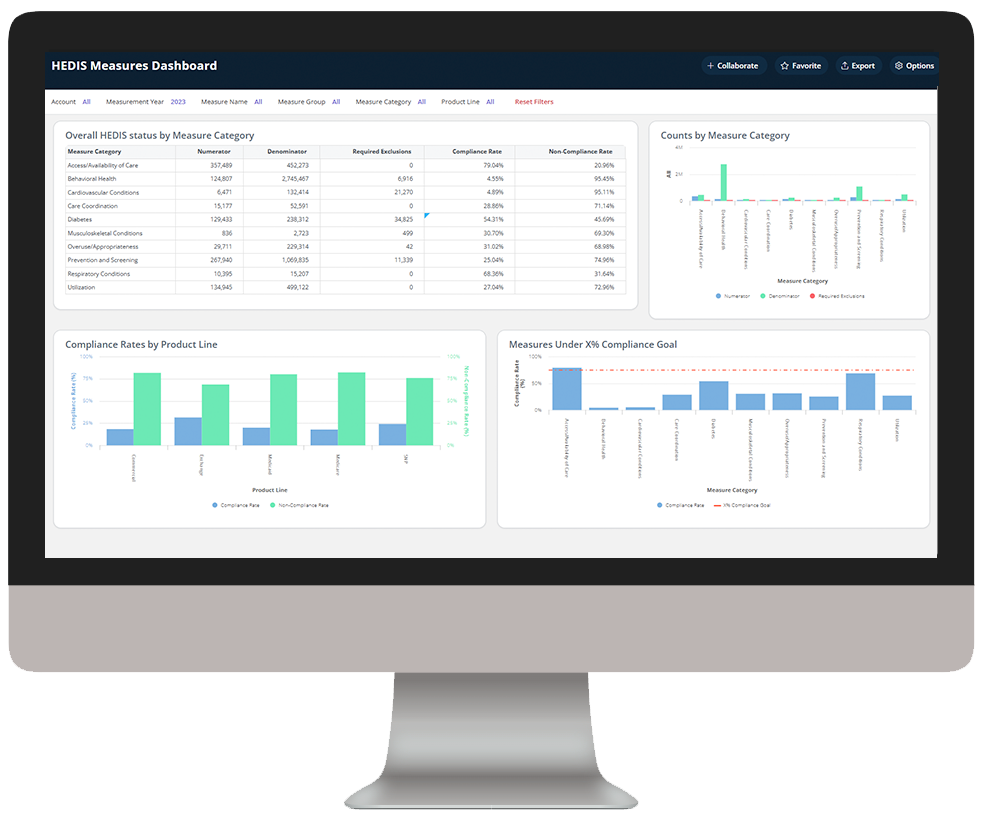
Assess HEDIS measure performance and compliance
Dive deeper into Quality Insights
Download the data sheet to see how Quality Insights can help your health plan improve care quality and outcomes.
Visit our Value-Based Care Blueprint page for everything you need to know to navigate the intersection of value and analytics.
Get our take on industry trends
The future of digital health part 3: AI, machine learning and robotics
This post is part three of a new series featuring healthcare visionary and thought leader Andy Dé. In this series, Dé discusses how COVID-19 has triggered remarkable digital transformation and uncovers five, long-term innovation implications that providers, healthcare leaders, and payers need to consider.
Read on...The future of digital health part 2: Digital patient engagement and virtual healthcare delivery
Protecting the health, well-being and safety of healthcare practitioners and first responders is paramount — and will accelerate adoption of Digital Patient Engagement (DPE), enabled by Virtual Healthcare Delivery (VHD) solutions (also known as “Hospital at Home.)”
Read on...Gamification in healthcare only works if you can measure it – here’s how
In business and in sports, it’s all about teams. What teams can accomplish when they work together. How they can fail spectacularly when they do
Read on...Pandemic fuels 2021 healthcare megatrends
When I wrote about megatrends last year, the predictions were, naturally, forward-looking. Telehealth, for example, was important because of increased healthcare consumerism and the convergence of technologies to make its use quick and easy for payers, providers and patients.
Read on...Want to talk with one of our experts?
Payer Value Analytics: Our full lineup of payer solutions
Everything you need to step into the future of healthcare and drive real change across populations.
Quality Insights
Activate insights into population health and quality to improve satisfaction and outcomes for members and maintain a competitive position in the market.
Employer Insights
Elevate data sharing with employer groups to demonstrate plan value and increase efficacy of risk stratification and care management plans.
Network Insights
Accelerate provider performance with evidence-based outcomes comparisons, cost-effectiveness analyses, and extensive segmentation capabilities.