Integrated Patient Insights
Focused and curated patient insights at the point of care
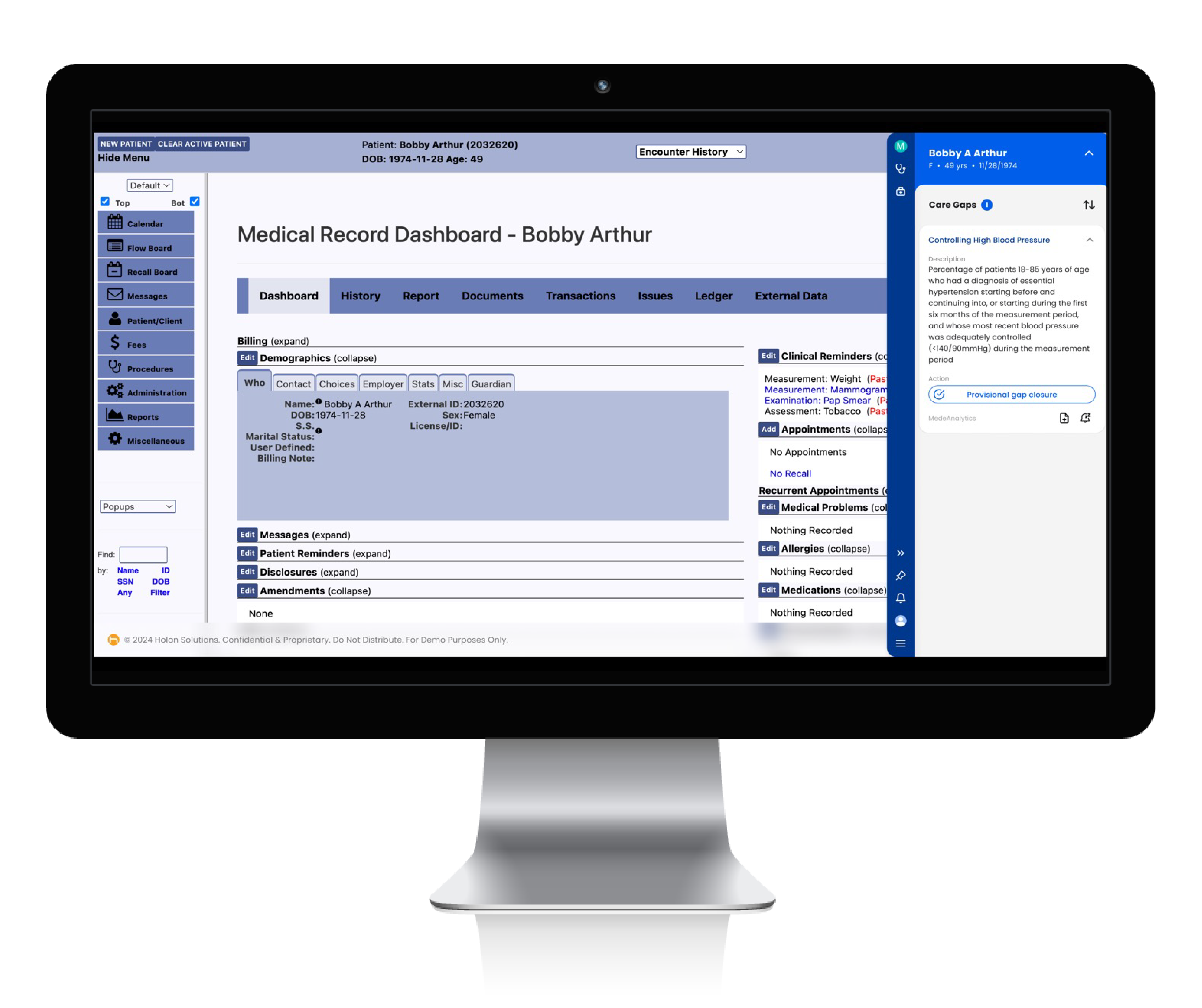
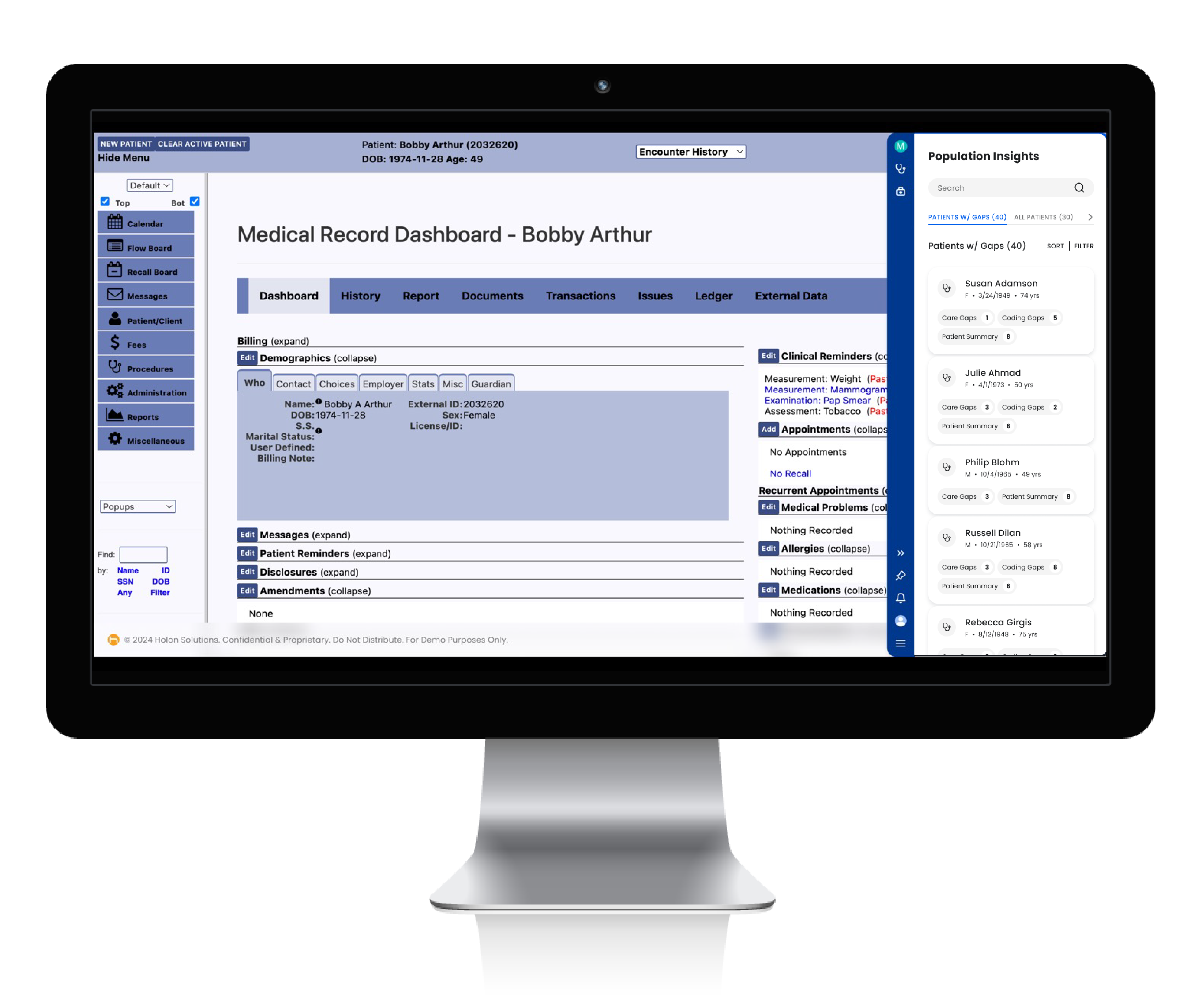
Integrated Patient Insights (IPI) revolutionizes healthcare delivery by providing real-time access to critical patient information at the point of care. This innovative solution empowers healthcare providers with immediate insights into care gaps, coding discrepancies, population health data, and social risk factors.
By seamlessly integrating vital data into the patient care process, IPI enables swift, informed decision-making that significantly improves patient outcomes. This transformative approach paves the way for a more efficient, effective and economical healthcare delivery system, benefiting all stakeholders in the healthcare ecosystem.
Empower care teams to close gaps effectively, achieve performance targets, and improve overall outcomes
Challenge
Solution
Providers lack timely and relevant patient information at the point of care
Challenge
Solution
Care gaps that go unrecognized can lead to increased utilization costs, poor care management, and lower patient satisfaction
Challenge
Solution
Providers often don’t have all the information to accurately code for risk adjustment, resulting in inaccurate patient statuses and reimbursements
Celebrating advancements in Integrated Patient Insights
 With IPI, providers will see significant improvements in their operations and patient care quality. Results indicate an 80% increase in gap closure rates, a 5% improvement in revenue capture, and substantial time savings for care teams, allowing them to focus more on patient care and less on administrative tasks.
With IPI, providers will see significant improvements in their operations and patient care quality. Results indicate an 80% increase in gap closure rates, a 5% improvement in revenue capture, and substantial time savings for care teams, allowing them to focus more on patient care and less on administrative tasks.
This partnership between MedeAnalytics and Holon marks a significant step forward in activating additional value from quality solutions, such as Quality Insights and Social Risk Insights, to better drive provider engagement within value-based care. By bringing actionable analytics directly to clinicians during patient encounters, this partnership promises to provide a decisive edge for care teams and improve outcomes in real time.
Analytics in action
Integrated Patient Insights integrates directly with your existing workflows, pulling patient information from your EHR and other systems and delivering insights through a low-profile overlay on your EHR interface.
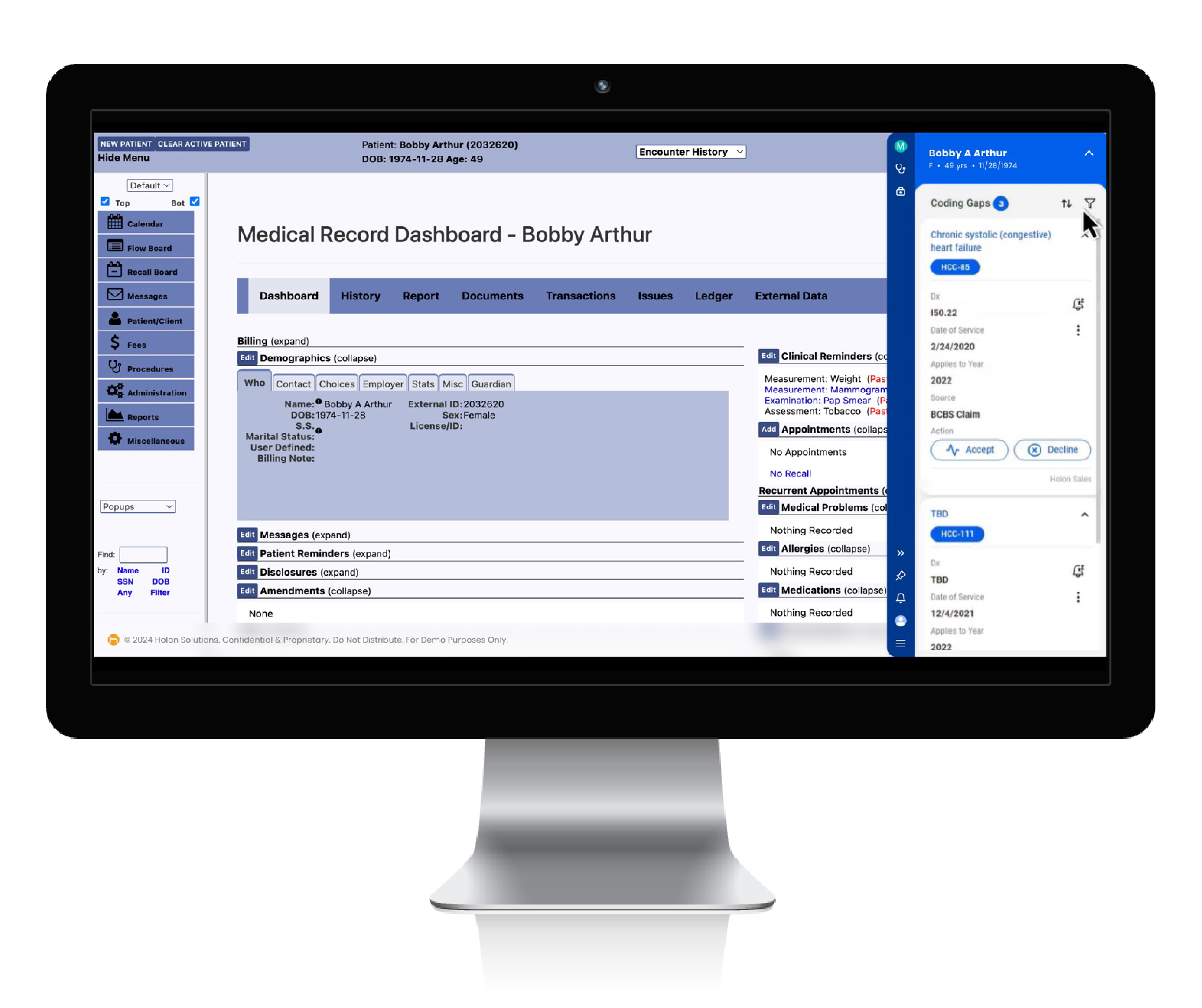
Coding gaps are presented in real time to the care team to accept or decline
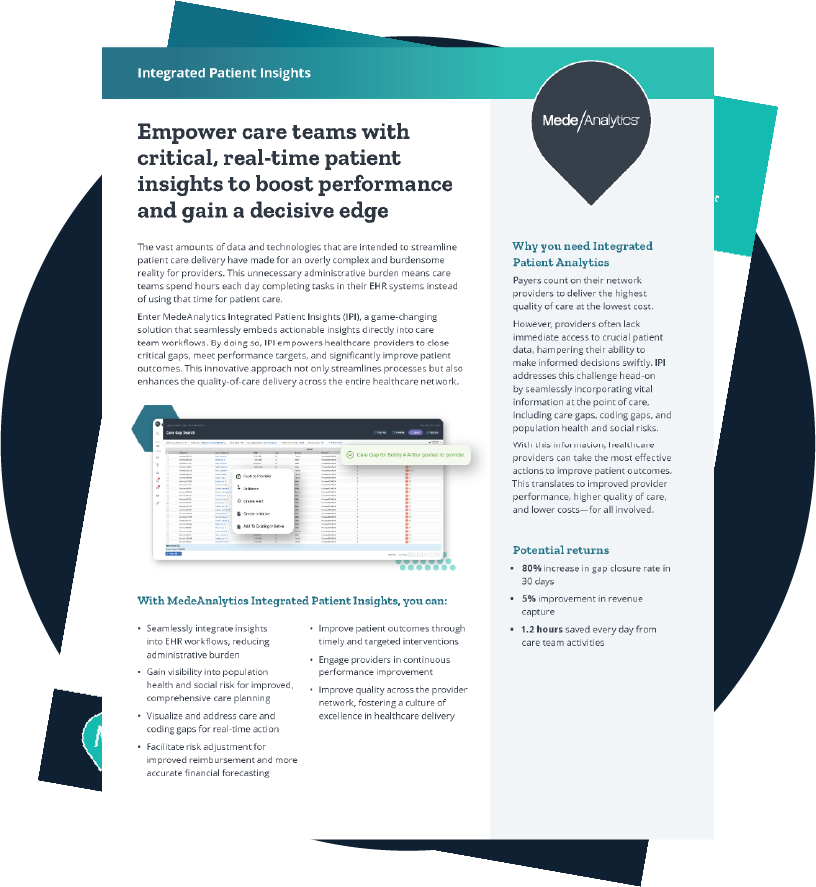
Dive deeper into Integrated Patient Insights
Download the data sheet to learn how Integrated Patient Insights can help healthcare providers take the most effective actions to improve patient outcomes, resulting in improved provider performance, higher quality of care, and lower costs for all involved.
Get our take on industry trends
Avoid COVID-19 modeling pitfalls by eliminating bias, using good data
COVID-19 models are being used every day to predict the course and short- and long-term impacts of the pandemic. And we’ll be using these COVID-19 models for months to come.
Read on...Population Health Amid the Coronavirus Outbreak
In speaking with many colleagues throughout the provider and payer healthcare community, I’ve found an overwhelming sense of helplessness to the outbreak’s onslaught. This is exacerbated by the constant evolution of reported underlying medical conditions that indicate a higher risk of hospitalization or mortality for a coronavirus patient.
Read on...3 Steps Any Healthcare Organization Can Take to Improve Enterprise Analytics
By Kristin Weir When it comes down to the most basic purpose of why organizations use analytics, it’s simple: they…
Read on...Why Predictive Analytics is the Answer to Healthcare’s Big Data Problem
By Scott Hampel Making improvements in healthcare data analytics has the potential to lead to significant cost savings and improved…
Read on...Want to talk with one of our experts?
We're driving data-powered improvement across the industry

Healthcare payers and health plans
Healthcare Payers and health plans
deploy our value-based care and provider network analytics to enhance population health, quality and network management and empower their employers and brokers through self-service analytics.

Healthcare providers and health systems
Healthcare Providers and Health Systems
use our end-to-end revenue cycle management analytics to lower denials, accelerate A/R, and improve staff productivity.

Government Medicare and Medicaid programs
Government Medicare and Medicaid programs rely on our comprehensive dashboards to understand cost drivers, gaps in care, and social determinants impacting beneficiary outcomes.