Part 3
This post is part three of a new series featuring healthcare visionary and thought leader Andy Dé. In this series, Dé discusses how COVID-19 has triggered remarkable digital transformation and uncovers five, long-term innovation implications that providers, healthcare leaders, and payers need to consider.
The past two weeks, Dé led us through the first two implications (you can catch up part 1 and part 2 ), and today he dives into today he dives into numbers three and four.
Innovation implication #3: Artificial intelligence and machine learning for operations, revenue cycle and supply change management innovation
There is a growing need to enable advanced predictive, prescriptive and spatial analytics to empower executives, line of business (LOB) leaders, clinicians and nurses at the point of care. As a result, we’re seeing a convergence of AI (machine learning, deep learning, natural language processing) and descriptive and spatial analytics with actionable, forward looking insights to power critical decisions.
I predict health systems and hospitals leveraging these advanced technologies and analytics for operations, revenue cycle and supply chain innovation to:
- Locate and design new facilities, testing centers and supply chain warehouses
- Optimizes access to care and convenience for patients and their families
- Expands capacity for cardiovascular procedures, hip and knee replacements, cancer care and more, with the ability to align capacity with demand
- Optimize supply chain network (especially for overseas suppliers)
- Enables accurate and reliable demand forecasts
- Supports potential partnerships with Emergency Response Inventory Services Providers to ensure ample supply of N-95 masks, PPE, ventilators, testing equipment and supplies, critical therapeutics and vaccines, and medical devices and equipment
- Forecast demand for elective procedures and services from their patient population
- Leverages clinical, financial and socio-economic determinants of health data
- Accounts for hospital and provider capacity, as well as profitability from a revenue and margin perspective
- Prioritizes treatment and services at hospital locations aligned with that demand for optimal patient access
Innovation implication #4: Medical robotics
I expect visionary leaders at top healthcare organizations and health systems to embark on a journey to embrace medical robotics. Robotics can enable process automation and higher efficiencies while assuring safety for healthcare personnel and front-line workers.
The framework below shows four primary areas and corresponding applications that are already being enabled by robotics – and will continue to be developed and explored in the post-pandemic era.
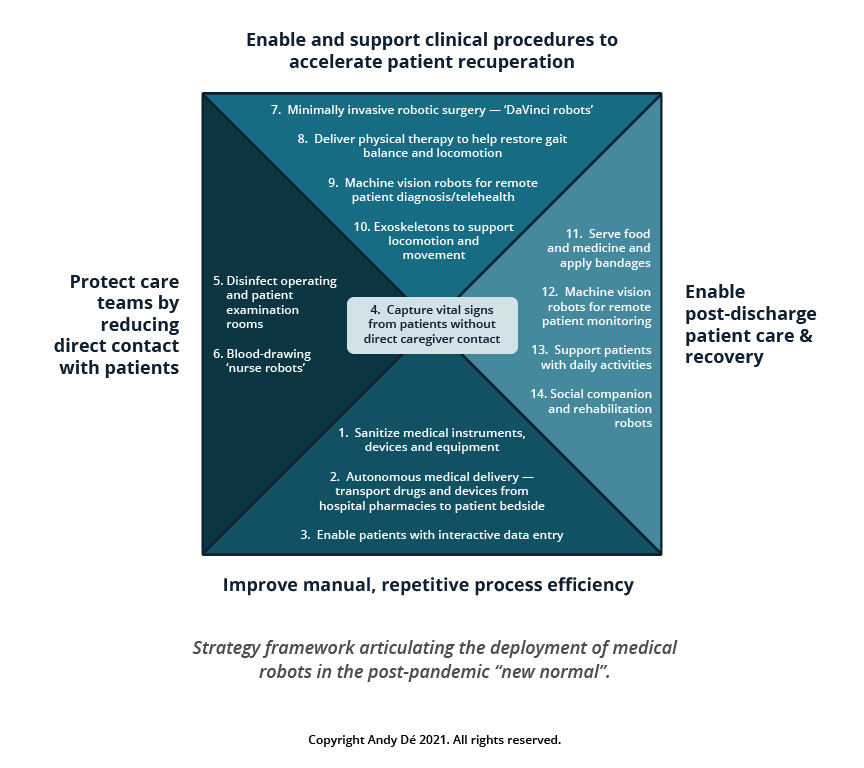
Countries including Japan, China, South Korea, and Taiwan are already testing the use of multiple applications ranging from improvement of manual process efficiency to protection of care teams through non-contact diagnosis enablement and support of clinical procedures to enabling post-discharge patient care and recovery.
That wraps up our dive into AI, machine learning, and robotics. Tune in next week for our fifth and final innovation implication: convergence of AI and analytics for healthcare payers. If you have any questions about what I’ve covered in this series so far, don’t hesitate to reach out.
Get our take on industry trends
You’re asking too much of your EHR
Electronic Health Records (EHRs) are purported to do a lot of things to support healthcare providers, and most of their claims are generally accurate. Of course, like anything, there are many areas where EHR vendors could and should make improvements.
Read on...Gamification in healthcare only works if you can measure it – here’s how
In business and in sports, it’s all about teams. What teams can accomplish when they work together. How they can fail spectacularly when they do
Read on...Pandemic fuels 2021 healthcare megatrends
When I wrote about megatrends last year, the predictions were, naturally, forward-looking. Telehealth, for example, was important because of increased healthcare consumerism and the convergence of technologies to make its use quick and easy for payers, providers and patients.
Read on...Measuring provider cost and utilization
No matter the time of year, payers and providers should work to agree on a shared source of truth when it comes to data. With the recent end of the year, it’s time to celebrate the new year (who isn’t ready to say goodbye to 2020?) and close the books, which includes the reconciliation of any shared savings or losses.
Read on...



