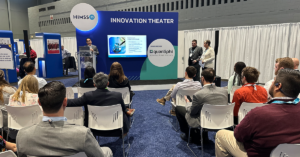
Our own Dave Schweppe (Chief Analytics Officer) and David Wolf (AVP, Payer Solutions) sat down with Todd Sauers, Manager of Value-Based Care Analytics at Sentara Health, for a fireside chat to discuss current trends and opportunities in value-based care. In this vibrant conversation, the experts talked through various perspectives and thoughts on the impact of COVID-19 on clinical risk adjustment, the future of payer involvement in care delivery, best practices for payer-provider partnership, and more. Read on for a quick look at a few of the key insights and watch the entire conversation below.
MedeAnalytics: Healthcare has suffered quite a bit from the COVID-19 pandemic. Quality measures, admissions, readmit rates, delayed treatment care…. the list feels endless. As a result, the data from 2020-2021 is skewed and will have an asterisk by it forever. Clinical risk adjustment, however, is a very important data point when it comes to value-based care; it’s basically a normative comparison across a population. So, when you look at the data and the unprecedented reduction of care in 2020, what do you think about your clinical risk adjustment process?
Todd Sauers, Sentara Health: We saw dramatically lower risk scores in 2020, and that bled into the beginning of 2021, too. We’re also seeing that skew our shared savings calculation.
As you mentioned our physician partners have lost a lot of revenue, and we’ve employed two main response strategies. First, we attempt to really limit the impact of what’s already happened. We decided we’re not paying out shared savings for 2020 alone; instead we’re extending and combining that performance period with 2020 and 2021 together. We’re also trying to avoid using those 2020 risk scores on their own. We’ve opted to look at blending 2020 with 2019 and 2021 to allow the more normal years to risk adjust that combined period.
Secondly, we are looking forward to limiting future impact. We’re working with physician partners to explore potential capitation models that would keep payments going to primary care, specifically if there was a similar event in the future. Fortunately, we are seeing a high volume of interest in that kind of shift from our biggest provider partners.
MedeAnalytics: When you think about delivering optimal care, what is the role of payer organizations? And how do you see that role changing over the next 5-10 years?
T. Sauers: The optimal care delivery model has to include a strong payer-provider partnership. To contribute meaningfully to that partnership, we as payers have to balance our dual responsibilities of (1) seeing clinical care, quality and cost from a client or patient perspective and (2) working with providers to develop and implement new technology, care paths, pharmaceutical treatments and more.
Over the next 5-10 years I think we are going to see a lot more of this dedication to working together for the good of patients and the industry at large. Risk-based contracts and value-based frameworks are already leading us that way – and as payers we will be increasingly vital in disseminating best practices and enhancing cohesion across our various stakeholders.
MedeAnalytics: Building on that, what are some key strategies you’ve noticed for building trust and collaboration in that payer-provider relationship?
T. Sauers: Great question; it’s easy to dream of a partnership but putting in the work to establish it is the real step forward. At Sentara, we share our data as openly as we can with our physicians, so they can access the information they need about the patients they’re caring for. We have weekly check-ins and collaborative sessions where we share screens, show demos of what they can do in the tool, and navigate any issues they’re having. A senior rep from MedeAnalytics also joins in to help answer questions and identify custom solutions to our unique needs.
MedeAnalytics: Looking out over the horizon, how can payers be most helpful in improving the overall health journey of patients and simplifying how they interact with the healthcare system?
T. Sauers: Payers have both broad and deep insight across large populations about longitudinal care – and we can leverage that to ensure that people are getting the right care at an affordable cost. This means viewing the patient as a whole person, not just a diagnostic event, and ensuring they have the preventative care, emergent options, remote monitoring for chronic illnesses, end-of-life support, etc. that they and their loved ones need.
Interested in learning more? Watch the entire Fireside Chat from our Impact Summit below.
Get our take on industry trends
Best practice tools to build an integrated approach to multimorbidity
The traditional model of treating single diseases no longer works. Data collected from 2016 to 2019 indicated that 32.9% of…
Read on...Will adopting a risk-based approach with augmented analytics support care gap closure?
A common challenge for healthcare systems is how to properly segment its patient populations based on risk profiles and co-morbidities. Doing this well ensures a high quality of care delivery and superior patient outcomes.
Read on...4 questions healthcare executives are asking about augmented analytics
At our annual Impact Summit, I had the privilege to talk about augmented analytics and address questions from healthcare executives—many…
Read on...