STAR scores are a critical component of success for Medicare Advantage Plans, MSSP and REACH ACOs, driving them to maximize the amount of shared savings realized and attract Medicare beneficiaries to enroll in high-quality care plans. In fact, plans with a STAR score of 4.0 or higher accounted for 71% of Medicare Advantage in 2023. Read this blog post to learn how telehealth fits into STAR ratings and explore how to optimize your telehealth processes for great STARs performance.
What are STAR scores/ratings?
STAR scores are based on a combination of HEDIS quality of care measures and CAHPS member satisfaction surveys. Commercial and Medicaid alternative payment arrangements also use quality-of-care scorecards to determine the level of shared savings that at-risk provider organizations receive.
How do organizations use STAR scores?
Integrated provider organizations use STAR performance as a measure of how well they are closing gaps in care and incorporating patient feedback to improve satisfaction.
Where does telehealth fit into STAR ratings?
CMS started allowing healthcare providers and health plans to submit telehealth visits as encounters during the COVID-19 pandemic to enable at-risk organizations to (a) improve compliance with HEDIS quality of care measures and (b) reduce volume of missed HCC conditions contributing to HCC risk scores. Though the pandemic has slowed, in 2023 CMS announced its continuing recognition of telehealth encounters for many HEDIS measures.
What can telehealth contribute to STAR ratings?
Now that we know telehealth truly isn’t going anywhere, it’s time to double down on the quality of care provided through virtual means. With telemedicine, providers and payviders can:
- Advance care accessibility and help close quality of care gaps, particularly for patients in remote areas or with mobility issues
- Encourage patients to attend regular follow-ups and timely interventions, contributing to better preventive care and quicker reactive interventions
- Get a comprehensive view of patient status and care pathways with integrated data and reporting from both virtual and in-person encounters
- Improve compliance with HEDIS measures
Let’s take a look at four examples.
1 – Telehealth to improve compliance
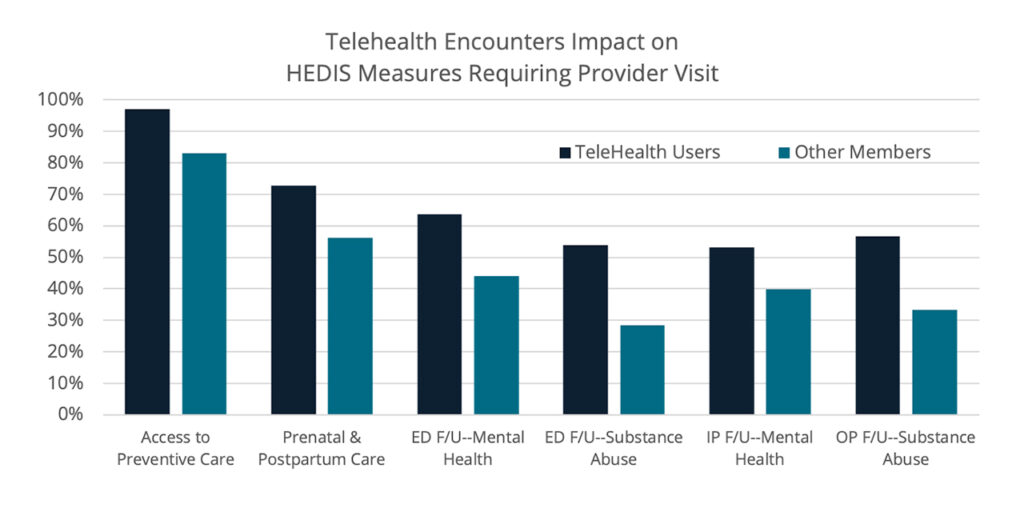
My team and I analyzed data from a sample of value-based risk organizations and discovered that members with telehealth encounters were more compliant resulting in higher HEDIS quality of care scores and STAR ratings.
Providers are using telehealth to increase compliance rates for measures such as:
- Post-emergency follow-up within 7 or 30 days after the visit for mental health and/or substance abuse issues, and multiple, high-risk, chronic conditions
- Post-hospitalization follow-up for mental health and/or substance abuse within 7 or 30 days after discharge
- Access to adult preventive care, well-child and adolescent preventive visits
- Timely prenatal and postpartum care for pregnant people
- Follow-up care for people prescribed ADHD medications;
- Cardiac rehabilitation
- Post-hospitalization follow-up for transitions of care
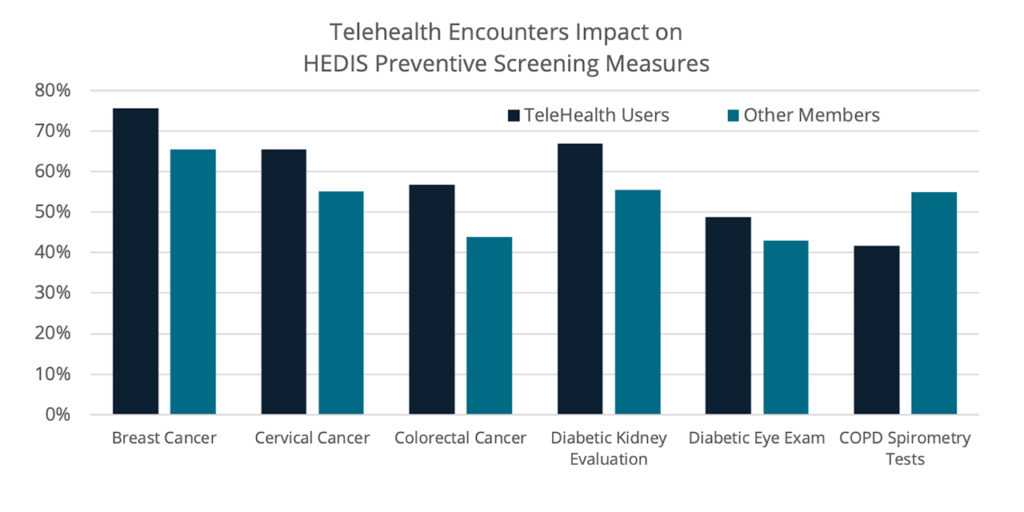
We also found that preventive care screenings are higher when members use telehealth to schedule necessary testing and/or review results of screening assessment with physicians for:
- Cancers—breast, colon and cervical cancer screenings
- Diabetics—eye exams and kidney health evaluations
- Care for older adults—functional and pain status assessments
- Depression screenings for at-risk populations
- Osteoporosis screenings for at-risk populations
In fact, spirometry assessments for people with COPD is the only measure we identified where people using telehealth showed lower compliance.
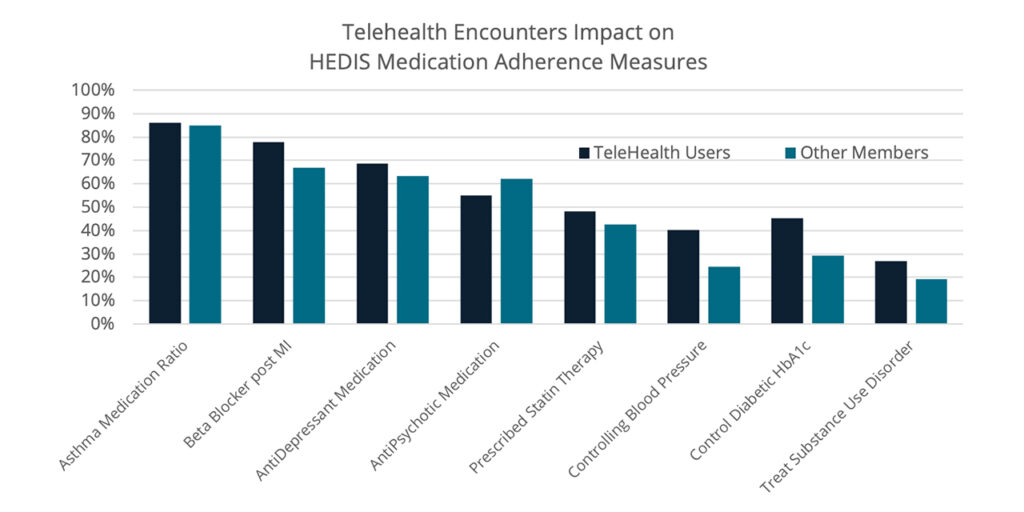
2 – Telehealth to manage medication adherence
Our analyses also showed that providers and payviders are using telehealth to fulfill evidence-based care guidelines for prescribing, administering and monitoring medication. This capability is especially important for patients/members who are receiving:
- Statin therapies prescribed for people with diabetes and cardiovascular disease
- Controlling blood pressure for people with diabetes and cardiovascular disease
- Persistence of beta-blocker therapy after a heart attack
- Controlling blood glucose (HbA1c levels) for people with diabetes
- Asthma medication ratio for inhaled corticosteroids
- Anti-depressants
- Antipsychotic medication adherence for people diagnosed with schizophrenia
- Treatment for substance use disorders
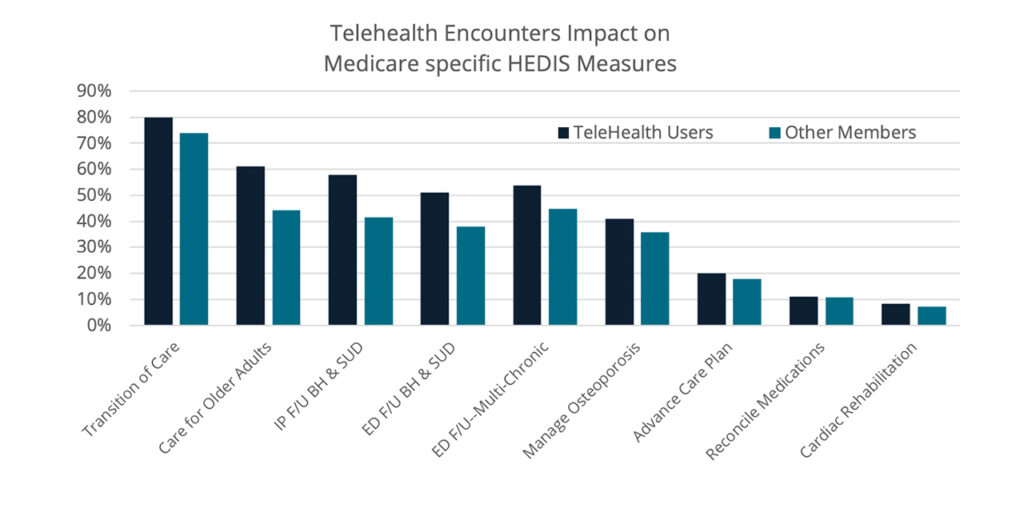
3 – Telehealth to facilitate care coordination
Telehealth can also be wielded powerfully to engage people that may be immunocompromised, have limited ability to travel, struggle with incapacitating mental health issues, or be nervous about attending in-person visits due to age or other identity factors. Technology-enabled care allows providers and payviders to meet the requirements of:
- Transition of care after discharge from inpatient hospital
- Medication reconciliation
- Follow-up within 30 days after ED visit or hospital discharge for older adults with multiple, high-risk chronic conditions, behavioral health issues, or substance abuse disorder
- Assessment of older adults’ pain and functional status;
- Advance care planning;
- Osteoporosis risk assessment and management;
- Cardiac rehabilitation after a cardiac event
4 – Telehealth to boost patient satisfaction
Telehealth also contributes to higher CAHPS patient satisfaction scores. One study found that patients reported significantly higher satisfaction with telemedicine visits, as compared with in-person visits, for surgical specialties, driven largely by significant differences in satisfaction among orthopedic surgery and general surgery.
In another recent publication, 97% of patients liked using telehealth for their physician visits, with 47% likely to request a telehealth visit in the future. Most patients appreciate the convenience of telehealth (97%) and 65-70% feel they received high-quality care and are comfortable with the treatment plan.
Patient satisfaction has been cited as the most integral element in the success of telemedicine implementation, adoption, and ongoing success.
Ready for more? Dig deeper on this topic.
Get our take on industry trends
Optimize your revenue cycle for today’s challenges and tomorrow’s goals
In this dynamic LinkedIn Live discussion, Christine Stetler, BSN, RN and AVP of Solution Engineering at MedeAnalytics, unearthed strategies for…
Read on...Enhancing healthcare delivery with explainable AI: A methodological leap forward
Healthcare providers and payers continually seek methods to enhance patient care and operational efficiency. With the advent of complex data…
Read on...Another year, another great HIMSS!
HIMSS24 was a fantastic event, as always. One of our favorite additions this year was the Digital Health Technology Theme…
Read on...Optimize your midcycle for telehealth services
Telemedicine is now a permanent fixture in homes across America. A majority of healthcare organizations have established the technology necessary…
Read on...



