A 2021 HFMA survey of health system executives found that 60% of providers are planning to move toward a “payvider” model in 2022 and take on a greater role in risk management. The survey also revealed that achieving strong data integrity and reporting tops the list of internal challenges health systems are facing as they take on more risk.
As the market optimizes for payvider adoption and growth, newly minted payvider organizations are looking to well-established veterans in the space for a blueprint of success. MedeAnalytics recently had the honor of co-hosting a Becker’s Hospital Review webinar with one of the most well-known large California payviders.
The webinar featured Kathryn Elder, Senior Consultant in National Customer Analytics & Reporting, and David Holt, Director of Underwriting, who discussed how the organization partnered with MedeAnalytics to drive success in data reporting, including:
- 75% reduction in turnaround times on ad-hoc reports for employers/brokers
- 80% reduction in turnaround times on ad-hoc reports for analysis and reporting
- Reduction in Pharma Rx costs by $4,000 per script through substitution of branded drugs with bio-similars (generics) that was rolled out nationally in under 24 months
- Return on investment/payback on MedeAnalytics solutions in just six months
So, how did they do it? And what has the impact been?
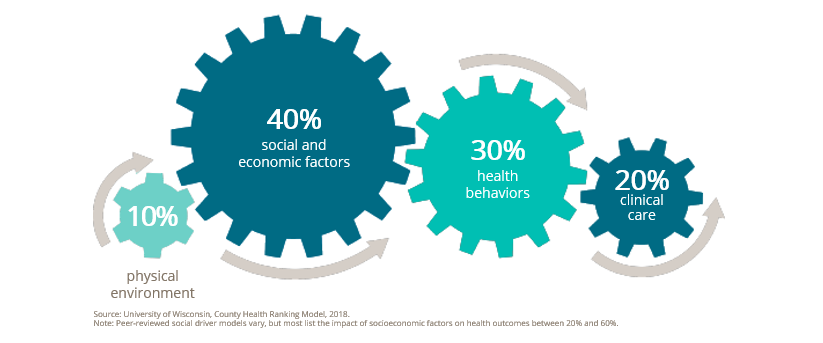
To start, they believe that ‘good health goes beyond healthcare.’ They strive to leverage information and resources to positively influence the major drivers of care shown below.
With that goal in mind, this large California payvider collaborated with MedeAnalytics to launch Analytic Insights. This initiative allowed the two companies to:
- Unify multiple, disparate data sources
- Create a single source of data truth with flexible, efficient reporting functions
- Launch a customizable suite of dashboards and reports, robust data analytics, industry benchmarks and more
- Assign appropriate roles and report access to clinical analysts and underwriters, salespeople, account managers and external brokers
- Gain the actionable data they needed to improve clinical engagement, community health and cost trends
In the webinar, they articulated seven (7) use cases summarized below:
- Integrating clinical and financial data via MedeAnalytics enables them to not only identify smokers but also quantify the cost and utilization of a smoker vs. non-smoker to help a customer implement a smoke free campus policy
- Similarly, the ability to identify adult Body Mass Index (BMI) prevalence rates and costs and stratify patient populations into risk-based segments or cohorts helped drive weight loss programs based on actionable data and insights
- Observation of lower rates of preventive care and COVID-19 vaccination rates helped target on-site education on preventive care and alternative ways to access care, impacting productivity for a mid-sized employer whose business model was based on commissioned sales and service.
- Analysis of pharmacy data via MedeAnalytics solutions helped this large California payvider identify a generic lower cost biosimilar drug resulting in a savings of $4,000 per script across all regions.
- Analysis of Opioid utilization at a customer identified increases in opioid utilization around one of the large state prisons as well as the network physicians responsible, culminating in a measurable reduction in opioid prescriptions.
- Given the needs of the underwriting department to ensure rate sufficiency for the upcoming contract period, proactively identifying high-cost claimants who are the largest driver of annual claims variation is critical. MedeAnalytics helped lower ad-hoc report turn-around-times (TAT) from weeks to minutes.
- Combining claims data with some clinical data (biometric, cancer screenings, chronic condition prevalence data) and comparing against their regional and industry benchmarks enabled its customers and brokers with self-service analytics, contributing to higher efficiencies, customer satisfaction and retention.
Elder and Holt identified five lessons learned that were critical to the success of this client's Analytics Insights:
- Set a clear vision and strategy with goals, objectives and metrics
- Secure executive buy-in and support from the beginning
- Build an ambassador network of experts and mentors to champion the solution and scale it with the business
- Prioritize education and training for internal and external stakeholders
- Engage with a software company with deep healthcare domain expertise who will partner with you for the long-term vs. a transactional relationship
As this exciting initiative continues to mature, we hope to keep enhancing analytical skills, capturing best practices, expanding clinical data sets, supporting customer engagement and accelerate self-service analytics adoption throughout the industry.
Watch the full webinar to see seven use cases demonstrating how we applied analytics to deliver evidence-based solutions and care to clients and patients respectively, while measurably improving efficiencies (75-80% reduction in analytic and reporting turn-around -times (TAT) while experiencing a 6-month payback on its MedeAnalytics solutions.
Get our take on industry trends
Why managed Medicaid/Medicare health plans need analytics to improve outcomes
Managed care organizations that provide healthcare services to Medicare/Medicaid members are dedicated to improving the health and wellness of these underserved populations, especially those living in rural areas.
Read on...Using consumer analytics to steer health-related decisions
Companies tap into what people like to eat and drink, how we purchase consumables, where we like to shop, what shows we might like to stream, whether we vote, and so on. If you have ever created a profile on a streaming application (think Netflix or Amazon), you will receive recommended books, movies and other items just as soon as you start surfing.
Read on...Run: Bringing Data Science into your Organization
In this three-part series, we’ve been detailing a tiered approach to introducing and incorporating data science into your organization. In Part One: Crawl and Part Two: Walk, we discussed how to get started from scratch and start building out a dedicated data science program. Today, we’ll dive into the third and final phase to see how to grow quality, centralize governance, incorporate user feedback, and more.
Read on...Walk: Bringing Data Science into your Organization
In this three-part series, we’re exploring a tiered approach to introducing and incorporating data science into your organization. In Part One: Crawl, we discussed how to get started from scratch. Today in Part Two: Walk, we’ll address issues that may emerge and how to overcome them, how to build out a dedicated data science team, and more.
Read on...


