
CDI Insights
Despite the widespread adoption of CDI programs, the revenue cycle is still hemorrhaging money. Over 80% of healthcare leaders recently reported inaccurate or insufficient clinical documentation as a primary contributor to this leakage. MedeAnalytics’ CDI Insights supports providers by delivering critical insights into documentation and coding performance—and offering paths to improvement.
Part of the Revenue Integrity Suite:
Drive claims accuracy to minimize denials and optimize reimbursement
Challenge
Solution
Complex, time-consuming reporting processes
Challenge
Solution
Limited visibility into problem areas for CDI team
Analytics in action
Our intelligent platform and intuitive user interface make it easy to unlock the value of your data. In as little as three clicks, we bring meaningful insights, powerful visualization, and analytics innovation to help you make an even bigger impact at your organization.
Explore a few key features by hovering over the image.
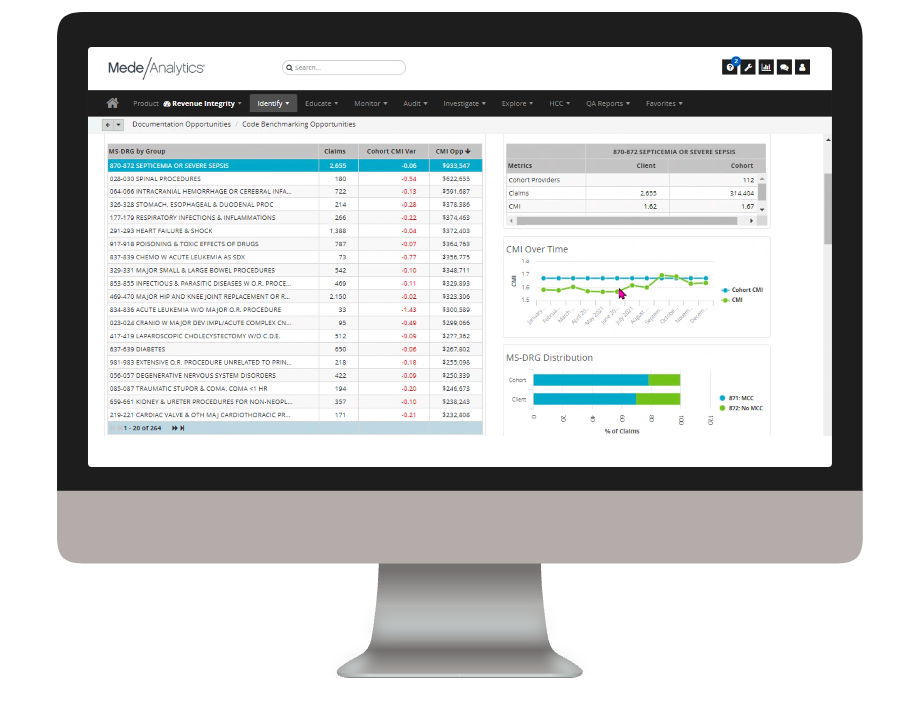
Quickly see CMI opportunity by MS-DRG
View your facility's CMI variance vs a cohort and what CMI opportunity you have for each MS-DRG
Trend your CMI over time and drill down to discover opportunities for improvement
Drill down to secondary diagnosis codes to find what secondary diagnosis you may be potentially under-coding vs. your cohort
Dive deeper into CDI Insights
Download the data sheet for next-level details about how CDI Insights can positively impact your financial and quality metrics—as well as patient outcomes.
Get our take on industry trends
Introduction to social risk: What healthcare leaders need to understand
‘Social determinants of health’ has been a common phrase for decades now, but the term social risk is much less…
Read on...AI is your new crystal ball: How predictive analytics can reduce denials
The idea of having a crystal ball to better understand what claims will be denied is an awesome concept. But one we can’t rely on. Thankfully, we have predictive analytics to take the place of a crystal ball.
Read on...3 ways to reduce friction in payer-provider relationships
The dynamic between healthcare providers and payers has historically been quite strained. Though both parties are interested in improving the…
Read on...Position your organization for success under CMS-HCC V28
The transition from CMS-HCC V24 to V28 heralds a significant shift in risk adjustment methodologies and emphasizes improved accuracy and…
Read on...Want to talk with one of our experts?
Provider Value Analytics: Our full lineup of provider solutions
Everything you need to support your front office, mid-cycle and back office.
Patient
Access
Insights
Optimize patient satisfaction during the patient registration and payment clearance processes with critical, real-time analytics information.
Revenue Integrity
Suite
See how clinical operations affect your bottom line with complete visibility into compliance risk and clinical documentation performance.
Business Office
Suite
Achieve optimized cash flow and operational excellence with big-picture insight into opportunities for improving collection rate, denials, and staff productivity.
Workforce Quality Insights
Use powerful analytics capabilities to generate end-to-end insights into how patient access activities are impacting the back-office outcomes.
Cost
Insights
Drill down into claims and encounter-level data to target and align controllable costs with outcomes and reimbursement.
Productivity
Analytics
Collect and deliver real-time insights on individual and collective registrar performance, and identify opportunities for training.









