
CDI Insights
Despite the widespread adoption of CDI programs, the revenue cycle is still hemorrhaging money. Over 80% of healthcare leaders recently reported inaccurate or insufficient clinical documentation as a primary contributor to this leakage. MedeAnalytics’ CDI Insights supports providers by delivering critical insights into documentation and coding performance—and offering paths to improvement.
Part of the Revenue Integrity Suite:
Drive claims accuracy to minimize denials and optimize reimbursement
Challenge
Solution
Complex, time-consuming reporting processes
Challenge
Solution
Limited visibility into problem areas for CDI team
Analytics in action
Our intelligent platform and intuitive user interface make it easy to unlock the value of your data. In as little as three clicks, we bring meaningful insights, powerful visualization, and analytics innovation to help you make an even bigger impact at your organization.
Explore a few key features by hovering over the image.
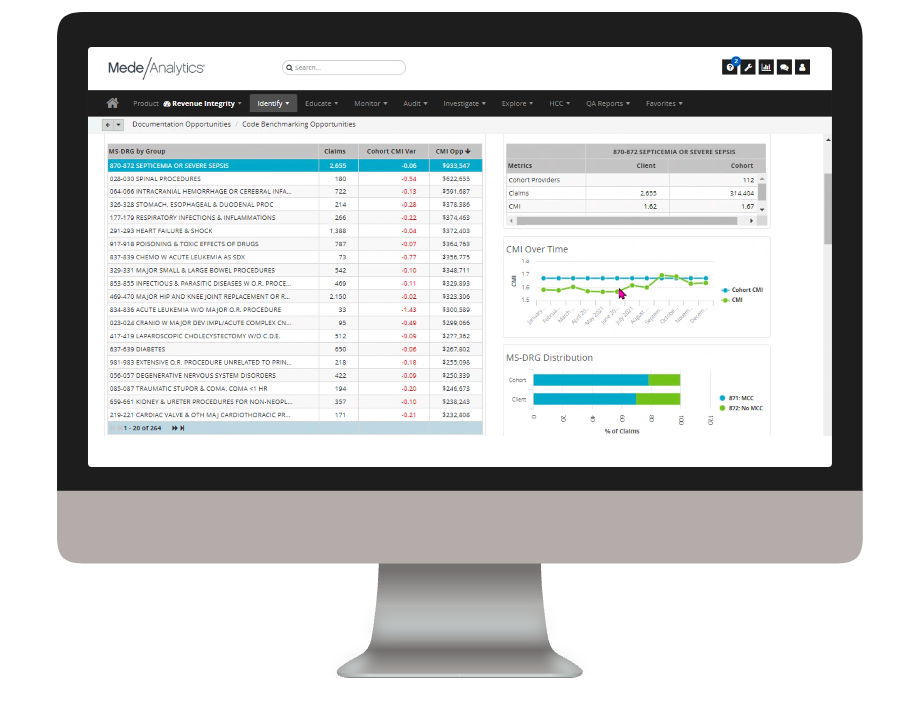
Quickly see CMI opportunity by MS-DRG
View your facility's CMI variance vs a cohort and what CMI opportunity you have for each MS-DRG
Trend your CMI over time and drill down to discover opportunities for improvement
Drill down to secondary diagnosis codes to find what secondary diagnosis you may be potentially under-coding vs. your cohort
Dive deeper into CDI Insights
Download the data sheet for next-level details about how CDI Insights can positively impact your financial and quality metrics—as well as patient outcomes.
Get our take on industry trends
Measuring provider cost and utilization
No matter the time of year, payers and providers should work to agree on a shared source of truth when it comes to data. With the recent end of the year, it’s time to celebrate the new year (who isn’t ready to say goodbye to 2020?) and close the books, which includes the reconciliation of any shared savings or losses.
Read on...Data visualization: A picture is worth a thousand…healthcare data points?
The amount of data produced daily has grown exponentially with nearly 90% of the world’s data generated in the last two years alone. To ensure we can make sense of this data, analysts must find meaningful ways to present the information to their audiences.
Read on...Crystal ball not necessary: predictive analytics helps health systems reduce denials
The idea of having a crystal ball to better understand what claims will be denied is an awesome concept. But one we can’t rely on. Thankfully, we have predictive analytics to take the place of a crystal ball.
Read on...How did we get here? Hospital analytics and the new normal
I have heard the word “unprecedented” so many times in 2020 that it has lost its significance; many of us have become desensitized to the extraordinary changes in the world this year.
Read on...Want to talk with one of our experts?
Provider Value Analytics: Our full lineup of provider solutions
Everything you need to support your front office, mid-cycle and back office.
Patient
Access
Insights
Optimize patient satisfaction during the patient registration and payment clearance processes with critical, real-time analytics information.
Revenue Integrity
Suite
See how clinical operations affect your bottom line with complete visibility into compliance risk and clinical documentation performance.
Business Office
Suite
Achieve optimized cash flow and operational excellence with big-picture insight into opportunities for improving collection rate, denials, and staff productivity.

Workforce Quality Insights
Use powerful analytics capabilities to generate end-to-end insights into how patient access activities are impacting the back-office outcomes.
See the solution ❯
Cost
Insights
Drill down into claims and encounter-level data to target and align controllable costs with outcomes and reimbursement.








