Mission critical emergency departments (EDs) are the most valuable revenue generating asset for hospitals. While visits decreased during the pandemic, hospitals are starting to report a return to nearly pre-pandemic levels. In December of 2022, more than 80% of hospital beds were in use nationwide, jumping 8 percentage points in two weeks. However, capacity varies across the country and changes day to day as hospitals have to adjust their bed availability due to staffing shortages and accessible resources. Using augmented analytics to predict ER visit trends can have a significant impact for hospitals and patients.
Business Challenge:
Given the staffing and resource challenges, reducing unnecessary emergency department (ED) visits should be a goal of all healthcare organizations. Unnecessary ED visits burden the healthcare system. They are costly and consume resources that other individuals with more acute needs may require. Additionally, unnecessary ED visits disrupt the continuity of care and could cause duplication of services resulting in diminished health outcomes for the patient.
To proactively address these challenges, healthcare providers need to better understand their patient populations, segment them based on risk, and address the reasons for which patients go to the emergency room. Health plans can also play a key role in managing ED visits by understanding and predicting ED visit trends and intervening early with education, physician incentives, and care management strategies for at-risk patients.
For non-emergent issues, the most common reasons relate to access: lack of a relationship with a primary care provider or care team, lack of after-hours or timely access to a provider, or barriers to access such as transportation. For other ED visits deemed avoidable, the reasons may be more complex, including inadequate chronic care management or gaps in care coordination among multiple locations of care.
Identifying patients who are already or could become ‘frequent flyers’ at EDs is always a good starting point. For instance, patients with type 2 diabetes on insulin who do not monitor their sugar with continuous glucose monitoring (CGM) will likely find themselves in this scenario time and again, which is completely avoidable. Understanding why they frequent the ED will potentially have the biggest impact on unnecessary ED utilization, improving asset utilization and ED revenues. Equally important is to stratify patients based on risk scoring using patient demographics, chronic conditions, medical or behavioral health issues (social determinants of health) and identify high and rising risk patients who are likely to visit the ED as a basis for reducing avoidable and unnecessary visits.
Augmented analytics, especially machine learning, deep learning and natural language processing (NLP), is a powerful tool that can be leveraged by providers and health plans to monitor, measure, analyze and reduce ED visits. If executed well, these can be strategically deployed to reduce unnecessary and avoidable ED visits, lower penalties and fines associated with 30-60-90 day re-admissions, improve ED asset utilization, and positively impact revenues while assuring superior patient outcomes.
Why augmented analytics is important:
Embedded augmented analytics capabilities are valuable tools in the healthcare industry for predicting ED visit trends and reducing avoidable emergent care. By providing timely insights into patient data, identifying patterns and trends, improving care coordination, and empowering patients, these solutions can help care managers improve patient outcomes, reduce healthcare costs, and improve the efficiency of the healthcare system.
For example, organizations can help identify patients who are at high risk of future ED visits. Using population health management dashboards, organizations can see a comprehensive view of ED utilization across an entire patient population, enabling care managers to identify trends and patterns that might indicate the need for targeted interventions. Care coordination tools can also be embedded into healthcare systems to improve communication and collaboration between different providers and care settings, ensuring that patients receive the right care at the right time and in the right setting.
Taking it a step further, linking with patient engagement tools can empower patients to take an active role in managing their health by providing access to health data, treatment options, and self-management tools. This approach can help reduce the likelihood of unnecessary ED visits by encouraging patients to take a more proactive approach to their health.
Essentially, embedded augmented analytics solutions can help healthcare systems and health plans identify patients who are at high risk of emergency room utilization and target interventions to reduce that risk. By improving patient outcomes, reducing healthcare costs, and improving the efficiency of the healthcare system, these solutions can have a measurable and positive impact on the healthcare industry.
What does this look like in practice: Proactively predicting ER visit trends for care managers to reduce emergent care
Proactively predicting ED visit trends for care managers involves using data analysis and predictive modeling techniques to identify high-risk patients who may require emergency care. By connecting data from electronic health records (EHRs), claims and clinical data, and other relevant sources, healthcare organizations can identify risk factors that contribute to increased ED visits, such as chronic conditions, demographic factors, and previous hospitalizations.
Once risk factors have been identified, healthcare organizations can leverage algorithms built into the analytics platform that can forecast future ED visits and assess which are potentially avoidable. Historical data can be used to train and test these models, and they can be adjusted over time as trends and new data emerge.
For example, ER diagnoses can be assigned a probability using four categories:
- Non-emergent
- Emergent/primary care treatable
- Emergent – ED care needed – avoidable
- Emergent – ED care needed – not avoidable
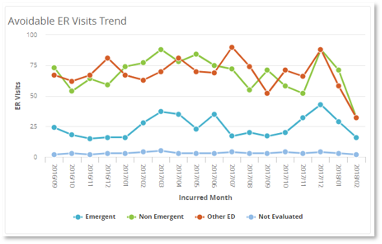
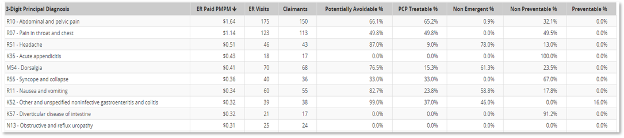
With this type of information, care managers can be armed with the necessary data to take a proactive approach to strategies tailored to the specific diagnoses of the patients. This may include regular check-ins, care coordination, and education to help patients manage their conditions and avoid emergencies. By intervening before an emergency occurs, care managers can reduce the likelihood of serious complications, improve patient outcomes, and enhance patient satisfaction by providing care in more convenient and cost-effective settings.
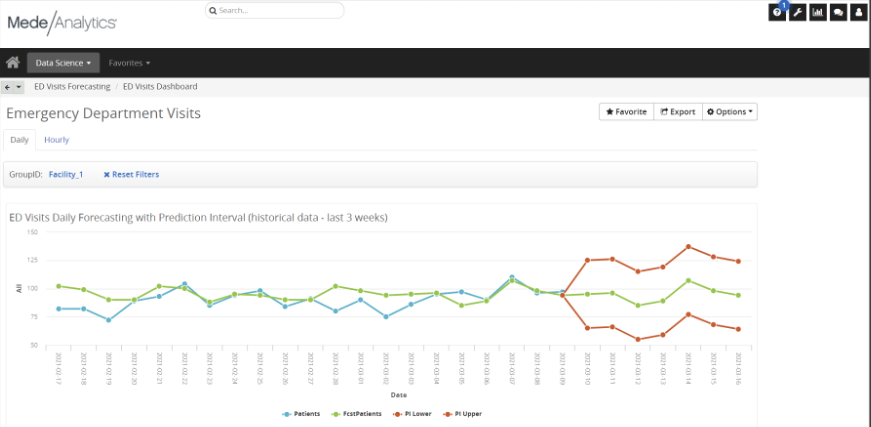
Reducing the number of unnecessary ED visits can also help healthcare organizations save money and allocate resources more efficiently. Emergency departments are often overcrowded and overburdened, and unnecessary visits can strain resources and reduce the quality of care for patients who truly need emergency services. By reducing the number of unnecessary visits, care managers can help optimize resource utilization and ensure that EDs are available for patients who truly need them.
In summary
The ability to proactively predict ED visit trends for care managers is a multi-step process that involves data analysis, predictive modeling, and care coordination. By identifying high-risk patients and intervening before an emergency occurs, care managers can improve patient outcomes, enhance patient satisfaction, and help healthcare organizations lower cost of care delivery while optimizing resource utilization.
Get our take on industry trends
The future of digital health part 3: AI, machine learning and robotics
This post is part three of a new series featuring healthcare visionary and thought leader Andy Dé. In this series, Dé discusses how COVID-19 has triggered remarkable digital transformation and uncovers five, long-term innovation implications that providers, healthcare leaders, and payers need to consider.
Read on...The future of digital health part 2: Digital patient engagement and virtual healthcare delivery
Protecting the health, well-being and safety of healthcare practitioners and first responders is paramount — and will accelerate adoption of Digital Patient Engagement (DPE), enabled by Virtual Healthcare Delivery (VHD) solutions (also known as “Hospital at Home.)”
Read on...You’re asking too much of your EHR
Electronic Health Records (EHRs) are purported to do a lot of things to support healthcare providers, and most of their claims are generally accurate. Of course, like anything, there are many areas where EHR vendors could and should make improvements.
Read on...Gamification in healthcare only works if you can measure it – here’s how
In business and in sports, it’s all about teams. What teams can accomplish when they work together. How they can fail spectacularly when they do
Read on...

