Cost Insights
Promote continuous improvement to elevate care and outcomes
Hospitals and health systems are strained from all angles with the pandemic decimating bottom lines. Protocols and pathways have failed to significantly reduce care variation—resulting in high levels of waste and unnecessary spending. Persistent inability to correlate treatment cost with quality of care has driven the cost of care delivery up without a measurable improvement in outcomes. If hospitals and health systems don’t take action to disrupt these ineffective processes, they will be in danger of bankruptcy within the next few years.
Delivering comprehensive solutions to lower your cost of care
Challenge
Solution
Ineffective data collection and analysis hinders ability to monitor, measure, analyze, and improve variances in modality utilization, procedures and supplies
Challenge
Solution
Lack of visibility into top and bottom performing service line and procedures.
Challenge
Solution
Limited integration capabilities with nationally accepted benchmarks and standards
Celebrating big wins with Cost Insights
Analytics in action
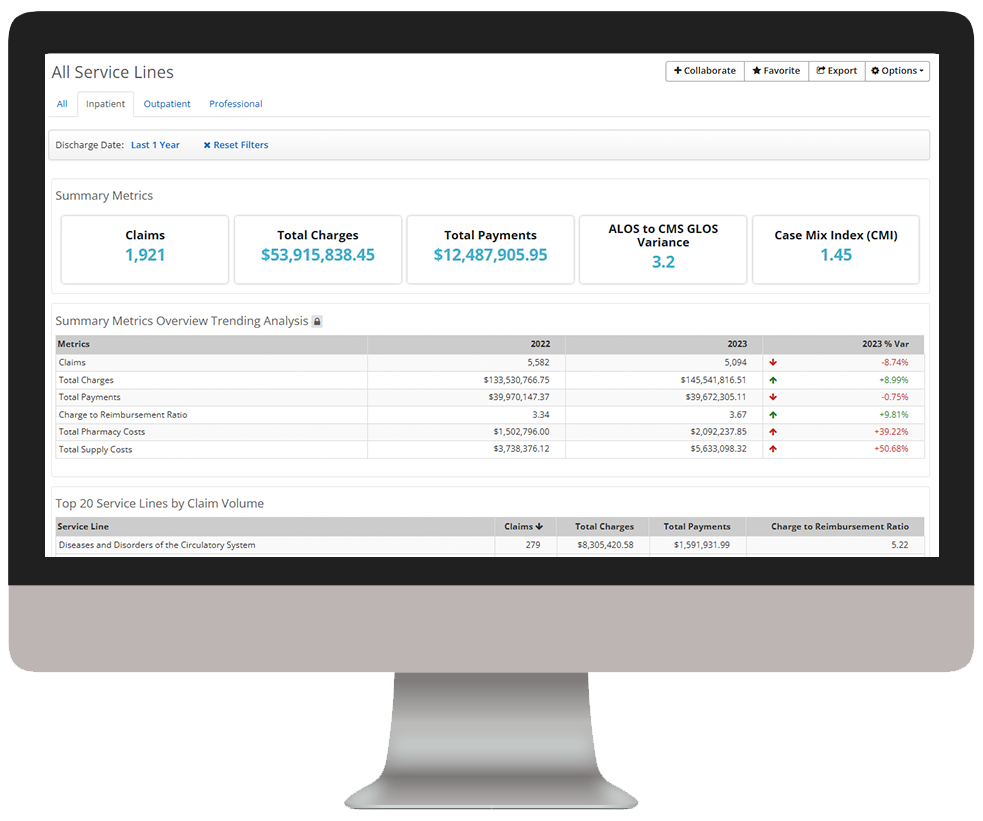
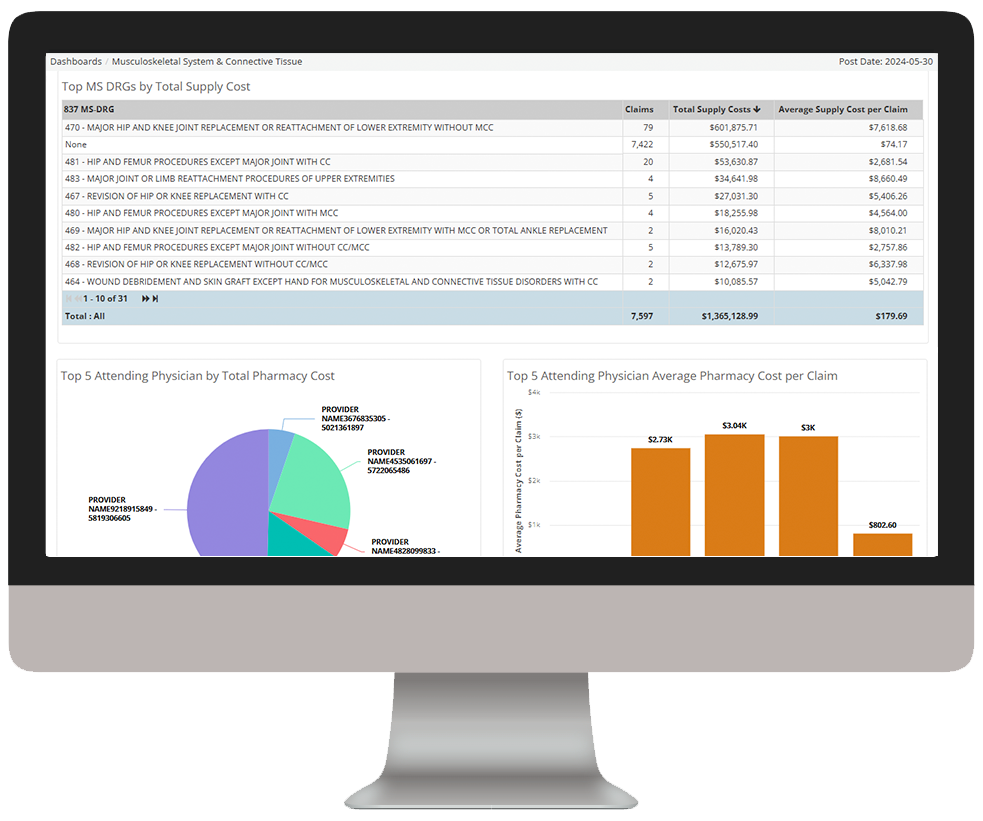
Our intelligent platform and intuitive user interface make it easy to unlock the value of your data. In as little as three clicks, we bring meaningful insights, powerful visualization, and analytics innovation to help you make an even bigger impact at your organization.
As you click through our example dashboards, hover over the image to explore a few key features.
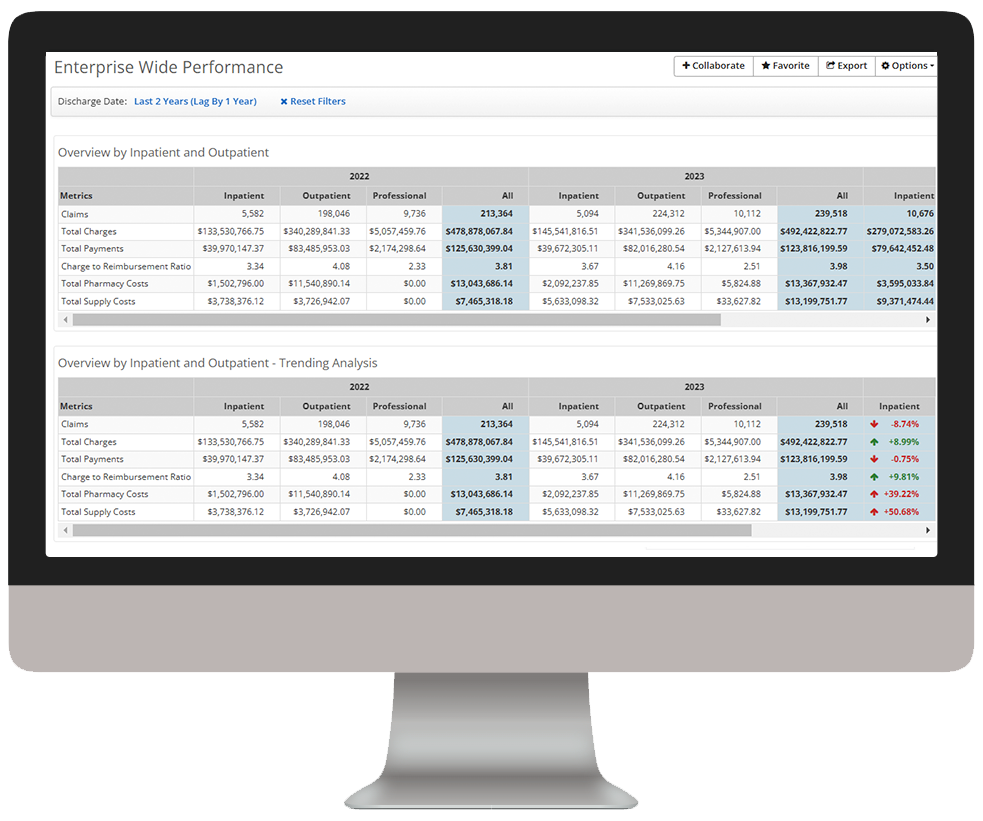
Get an enterprise-wide view of costs to identify opportunities for containment
Dive deeper into Cost Insights
Download the data sheet to see how Cost Insights helps you identify and act on direct cost of care improvement opportunities.
Get our take on industry trends
Five predictions for healthcare analytics and AI
Healthcare leaders increasingly realize the tremendous potential in artificial intelligence (AI) and analytics to deliver on the promise of high-quality…
Read on...Optimizing opportunity in value-based care
Our own Dave Schweppe (Chief Analytics Officer) and David Wolf (AVP, Payer Solutions) sat down with Todd Sauers, Manager of…
Read on...Want to talk with one of our experts?
Provider Value Analytics: Our full lineup of provider solutions
Everything you need to support your front office, mid-cycle and back office.
Patient
Access
Insights
Optimize patient satisfaction during the patient registration and payment clearance processes with critical, real-time analytics information.
Revenue Integrity
Suite
See how clinical operations affect your bottom line with complete visibility into compliance risk and clinical documentation performance.
Business Office
Suite
Achieve optimized cash flow and operational excellence with big-picture insight into opportunities for improving collection rate, denials, and staff productivity.

Workforce Quality Insights
Use powerful analytics capabilities to generate end-to-end insights into how patient access activities are impacting the back-office outcomes.
Cost
Insights
Drill down into claims and encounter-level data to target and align controllable costs with outcomes and reimbursement.
Productivity
Analytics
Collect and deliver real-time insights on individual and collective registrar performance, and identify opportunities for training.