Estimated reading time: 3 minutes
With most pregnancy-related deaths being considered preventable, why is the United States facing a maternal health crisis? The country’s maternal mortality rate is the highest of any developed nation in the world and more than double the rate of peer countries. Maternity-related issues are now more common in the public discourse thanks to social media platforms and brave women who are sharing their struggles. Inspired by these women, we dug a little further into the data to share ways that data analytics can offer insight and solutions for addressing this directly.
Who is the maternal health crisis affecting?
Each year, thousands of women experience unexpected outcomes of labor and delivery that result in significant short- or long-term consequences to their health. This can include heart issues, the need for blood transfusions, eclampsia, blood infections, and even death for the mother and child. These devastating outcomes are not new, but the COVID-19 pandemic has exacerbated them significantly.
Though these issues affect all pregnant women, socio-economic factors further impact maternal care and outcomes. Minoritized communities are faced with the most obstacles to receiving equitable care opportunities. Black women are three times as likely to die from pregnancy-related complications, and Native American women are more than twice as likely to die. Women who live in rural America — where there are many maternal care deserts — are about 60 percent more likely to die.
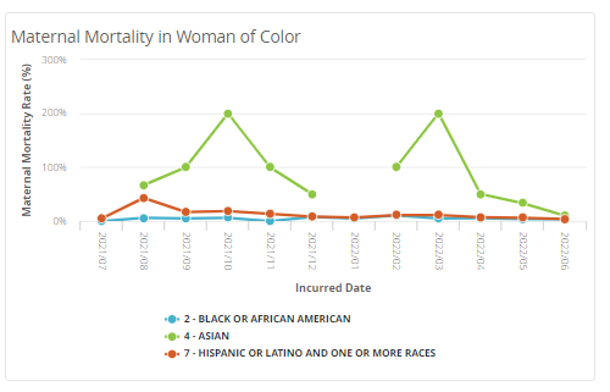
Specifically, the Medicaid population is disproportionately affected by the maternal health crisis, and Medicaid finances around 43% of all births in the United States.
What can health plans do to help solve this crisis?
In response to these issues growing in scope and visibility, federal and state governments have made maternal mortality a top priority to lower maternal mortality rates and reduce disparities. Health plans must play a major role in these initiatives given their proximity to and knowledge of the patient populations. To do so, they need data that tells a clear story and offers meaningful next steps.
Consider high-risk pregnancies, for example. Health plans empowered with advanced analytics can factor in pre-existing clinical conditions, race/ethnicity, and age to assess needs more thoroughly. The resulting insights can be used to collaborate with providers to drive early and ongoing interventions—and support healthy mom/baby programming.
Healthcare data can be hard to gather and harder to interpret—and that’s where data analytics can help.
Using analytics to combat this crisis:
Analytics must play a key part in the effort to minimize adverse outcomes with data insights. For example, using MedeAnalytics’ suite of maternal health modules and decades of public data, health plans can:
- Use fact-based data points to inform better, more equitable plans for those most at risk
- More accurately predict and reduce unexpected outcomes
- Provide a healthier pregnancy experience
- Track and trend pre-term births at the member and practice level to identify which practices need facilitation assistance
- Use month-to-month HEDIS prenatal and postpartum visits and postpartum depression screening data to drive quality improvement interventions and performance tracking

For Medicaid plans in particular, maternal health is the next frontier of care management. Especially from a health equity lens, health plans need an avenue to address the maternal care crisis and improve outcomes for mothers and their babies. Analytics can offer a common platform for health plans, providers, and members to work together to reduce health disparities and achieve longer-term improvements in women’s health.
Get our take on industry trends
Best practice tools to build an integrated approach to multimorbidity
The traditional model of treating single diseases no longer works. Data collected from 2016 to 2019 indicated that 32.9% of…
Read on...Will adopting a risk-based approach with augmented analytics support care gap closure?
A common challenge for healthcare systems is how to properly segment its patient populations based on risk profiles and co-morbidities. Doing this well ensures a high quality of care delivery and superior patient outcomes.
Read on...4 questions healthcare executives are asking about augmented analytics
At our annual Impact Summit, I had the privilege to talk about augmented analytics and address questions from healthcare executives—many…
Read on...