Watch the webinar
A central tenet of CalAIM is providing more equitable, coordinated and person-centered care. To achieve this, payers need access to data and tools to understand all the levers affecting beneficiary health and address the inequities that can result in better care quality and outcomes.
In this webinar, two industry experts shared their perspectives and best practices on:
- Payers and providers holding each other accountable for equity
- Leveraging data to foster the quality and effectiveness of care
- Ensuring equal and unrestricted access to behavioral, physical and social health care
This session focuses specifically on actionable strategies for California health plans, as CalAIM is currently the largest state-wide effort toward whole-person care.
What is CalAIM?
California Advancing and Innovating Medi-Cal — known as CalAIM — is a far-reaching, multiyear plan to transform California’s Medi-Cal program and integrate it more seamlessly with other social services.
Led by California’s Department of Health Care Services, the goal of CalAIM is to improve outcomes for the millions of Californians covered by Medi-Cal, especially those with the most complex needs. CalAIM will offer Medi-Cal enrollees coordinated and equitable access to services that address their physical, behavioral, developmental, dental, and long-term care needs, throughout their lives, from birth to a dignified end of life.

How can California MCOs successfully adjust and advance?
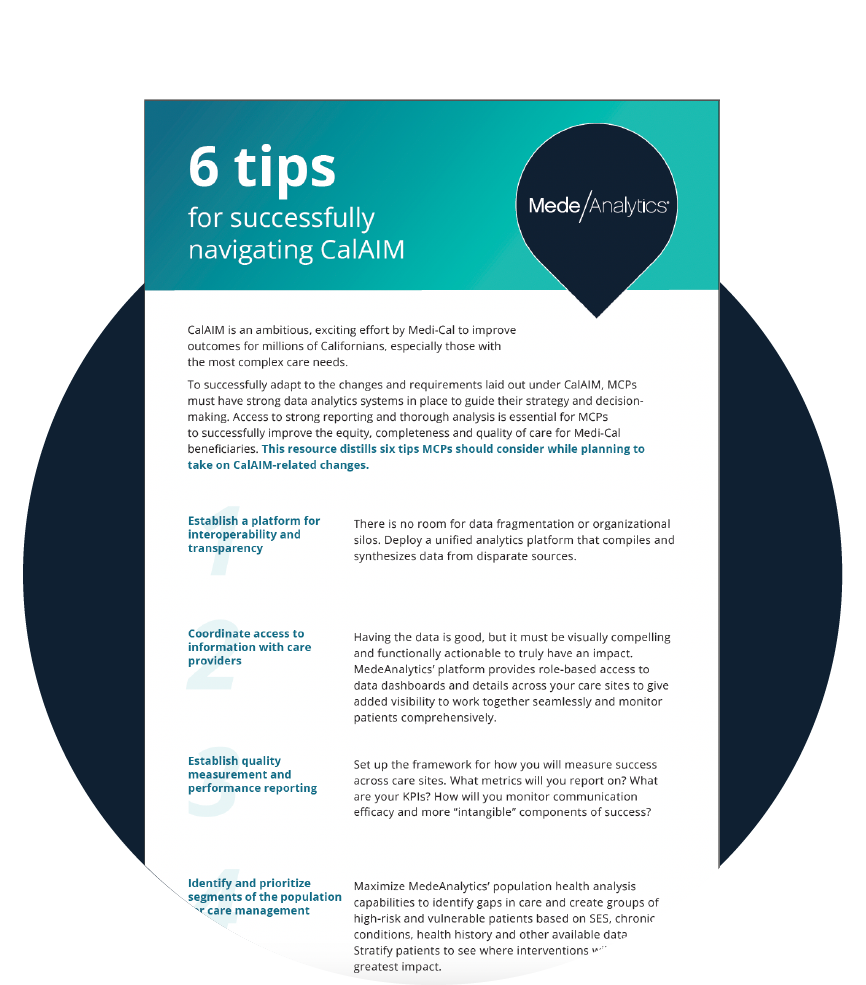
To successfully adapt to the changes and new requirements laid out under CalAIM, MCOs must have robust, accurate data. Access to strong reporting and thorough analysis is essential for MCOs to successfully improve the equity, completeness, and quality of care for Medi-Cal beneficiaries.
MCOs will need to:
- Ensure access to data and analytics
- Lay the groundwork for interoperability
- Establish transparency and accountability across care settings
Read on or check out our resources to learn how.
How are other payers transforming patient outcomes?
One client — a west coast payvider delivering high-touch, individualized care—came to MedeAnalytics with a few key goals:
- Address vulnerable populations
- Reduce hospitalizations for target groups
- Segment population groups for effective care management
Using MedeAnalytics’ Population Health solution, this client grew analytics and reporting capabilities, including determining "impactable" populations for interventions, aggregating data for patient stratification and cost analysis, and obtaining actionable insights about vulnerable patient populations. With predictive analytics, they were able to identify high-risk and rising-risk patients for in-home care delivery.
The organization realized incredible return on their analytics investment, ultimately creating significant impact across the organization, including:
How could MedeAnalytics help you?
Our dedicated, experienced team at MedeAnalytics can provide the foundation you need to align patient care across the continuum; identify and reduce health disparities; ease administrative burden and waste; and improve data-driven decision-making on population health strategy.
With MedeAnalytics platform, capabilities and commitment, MCOs benefit from data integration and transparency; identification and stratification of populations; quality measurement and performance reporting; and data security and role-based access.
Robust SDOH dashboards:
- Enable a detailed look at socioeconomic impacts on member care
- Inform outreach campaigns and care plans on environmental factors that have the most impact on outcomes of and/or access to care

What resources can help you along the way?
CalAIM can seem like a daunting endeavor. With the right tools and information, plans can start down the path to greater interoperability and deeper insights. We have assembled some resources that might be helpful along that journey.
California Health Care Foundation
Our journey to a healthier California for all
California Department of Health Care Services
Chat with an expert
© 2025 MedeAnalytics, Inc. All rights reserved | Terms of Use | Privacy Statement