Part 3
This post is part three of a new series featuring healthcare visionary and thought leader Andy Dé. In this series, Dé discusses how COVID-19 has triggered remarkable digital transformation and uncovers five, long-term innovation implications that providers, healthcare leaders, and payers need to consider.
The past two weeks, Dé led us through the first two implications (you can catch up part 1 and part 2 ), and today he dives into today he dives into numbers three and four.
Innovation implication #3: Artificial intelligence and machine learning for operations, revenue cycle and supply change management innovation
There is a growing need to enable advanced predictive, prescriptive and spatial analytics to empower executives, line of business (LOB) leaders, clinicians and nurses at the point of care. As a result, we’re seeing a convergence of AI (machine learning, deep learning, natural language processing) and descriptive and spatial analytics with actionable, forward looking insights to power critical decisions.
I predict health systems and hospitals leveraging these advanced technologies and analytics for operations, revenue cycle and supply chain innovation to:
- Locate and design new facilities, testing centers and supply chain warehouses
- Optimizes access to care and convenience for patients and their families
- Expands capacity for cardiovascular procedures, hip and knee replacements, cancer care and more, with the ability to align capacity with demand
- Optimize supply chain network (especially for overseas suppliers)
- Enables accurate and reliable demand forecasts
- Supports potential partnerships with Emergency Response Inventory Services Providers to ensure ample supply of N-95 masks, PPE, ventilators, testing equipment and supplies, critical therapeutics and vaccines, and medical devices and equipment
- Forecast demand for elective procedures and services from their patient population
- Leverages clinical, financial and socio-economic determinants of health data
- Accounts for hospital and provider capacity, as well as profitability from a revenue and margin perspective
- Prioritizes treatment and services at hospital locations aligned with that demand for optimal patient access
Innovation implication #4: Medical robotics
I expect visionary leaders at top healthcare organizations and health systems to embark on a journey to embrace medical robotics. Robotics can enable process automation and higher efficiencies while assuring safety for healthcare personnel and front-line workers.
The framework below shows four primary areas and corresponding applications that are already being enabled by robotics – and will continue to be developed and explored in the post-pandemic era.
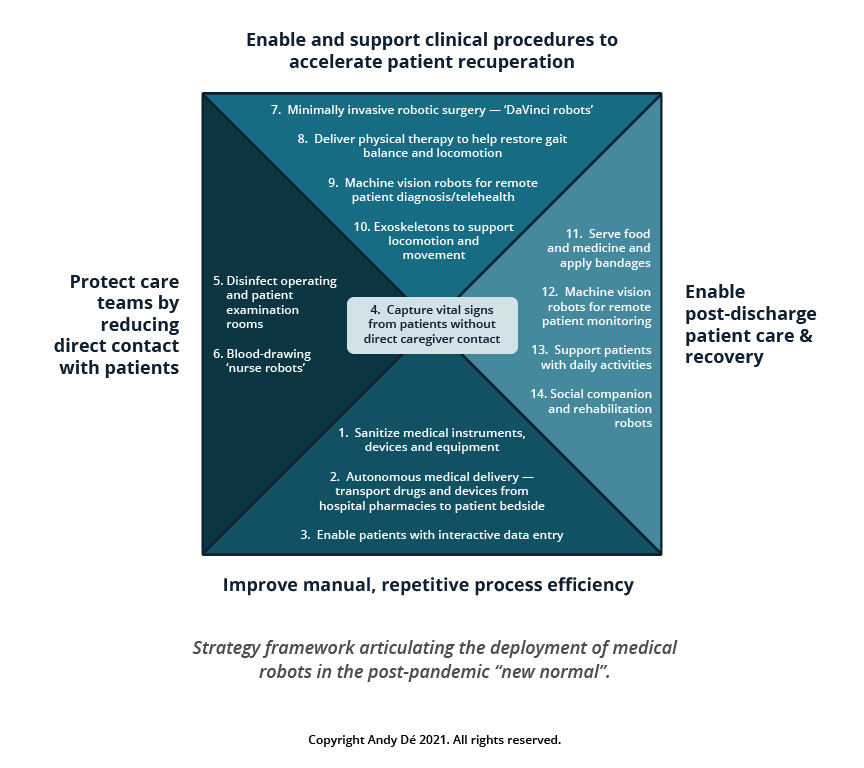
Countries including Japan, China, South Korea, and Taiwan are already testing the use of multiple applications ranging from improvement of manual process efficiency to protection of care teams through non-contact diagnosis enablement and support of clinical procedures to enabling post-discharge patient care and recovery.
That wraps up our dive into AI, machine learning, and robotics. Tune in next week for our fifth and final innovation implication: convergence of AI and analytics for healthcare payers. If you have any questions about what I’ve covered in this series so far, don’t hesitate to reach out.
Get our take on industry trends
Helping Accountable Care Organizations Navigate the Perfect Storm
In the ever-evolving landscape of healthcare, Accountable Care Organizations (ACOs) find themselves at the epicenter of a transformative era. Recently,…
Read on...Navigating the Medicare Landscape: Implications of the Latest Rule Changes for Healthcare Organizations
The Centers for Medicare & Medicaid Services (CMS) has recently unveiled significant proposed changes to Medicare Advantage (MA), Medicare Prescription…
Read on...Introduction to social risk: What healthcare leaders need to understand
‘Social determinants of health’ has been a common phrase for decades now, but the term social risk is much less…
Read on...AI is your new crystal ball: How predictive analytics can reduce denials
The idea of having a crystal ball to better understand what claims will be denied is an awesome concept. But one we can’t rely on. Thankfully, we have predictive analytics to take the place of a crystal ball.
Read on...



